Transforming medical equipment procurement globally

Why Hospital Equipment Procurement is a Strategic Priority for Modern Healthcare

Hospital equipment procurement is the systematic process of acquiring medical devices, technology, and supplies for healthcare facilities. It involves planning, vendor selection, purchasing, installation, and ongoing management of equipment essential for patient care.
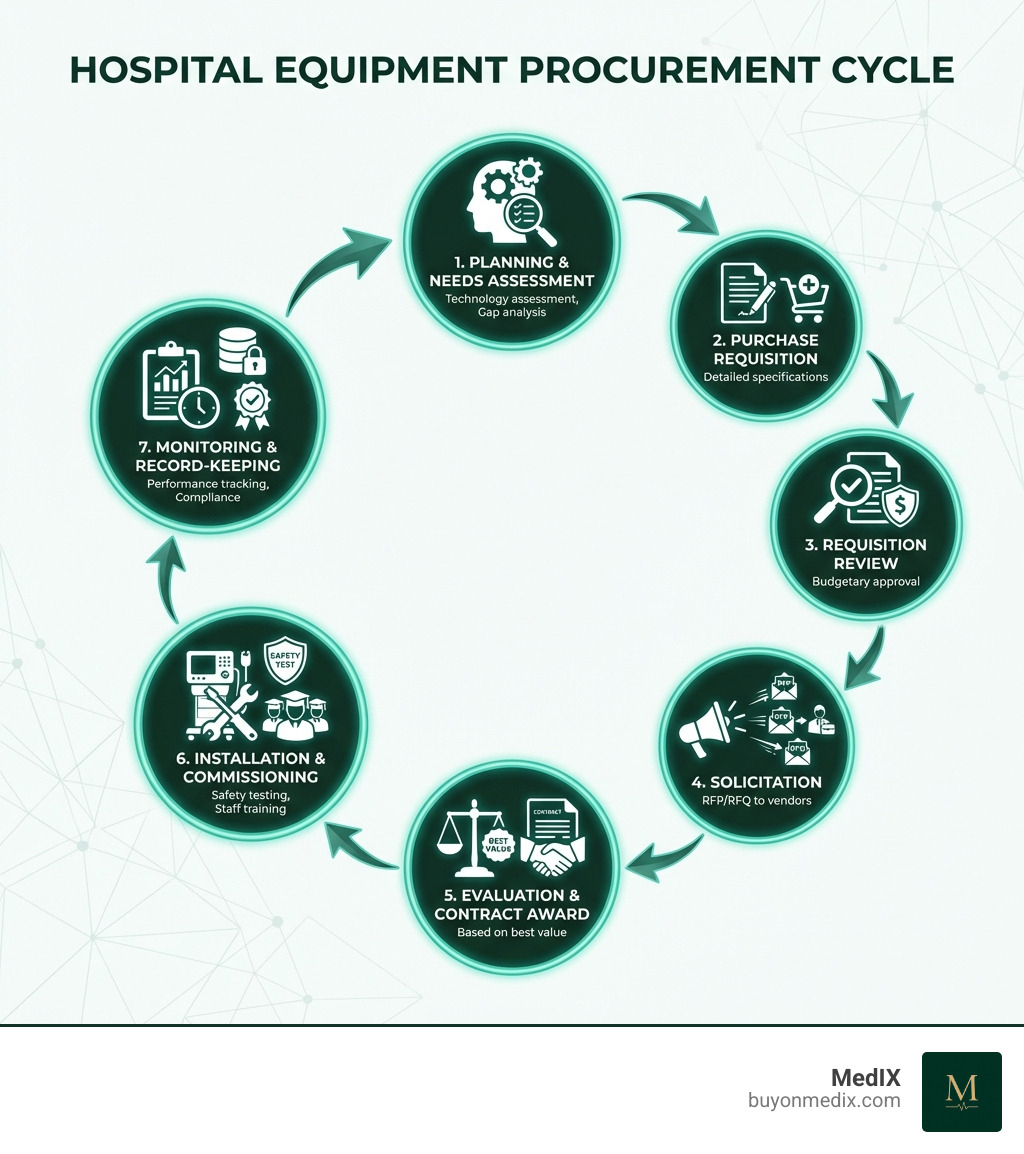
The Core Steps of Hospital Equipment Procurement:
- Needs Assessment - Identify equipment requirements and clinical gaps
- Technology Evaluation - Research devices, evaluate specifications, and assess total cost of ownership
- Requisition & Approval - Submit purchase requests and secure budget authorization
- Vendor Selection - Issue RFPs/RFQs, evaluate bids, and negotiate contracts
- Procurement - Place orders and manage contracts
- Installation & Commissioning - Prepare sites, install equipment, conduct safety tests, and train staff
- Monitoring & Record-Keeping - Track performance, manage maintenance, and maintain compliance documentation
Supplies represent the second largest cost to hospitals, trailing only human resources. Yet procurement often remains a fragmented, manual process in many healthcare organizations, despite rapid technological advancement in patient care itself.
Hospitals face a constant balancing act: delivering top-quality care while keeping costs under control. The stakes are high—poor procurement decisions can mean paying 20-30% more than necessary, dealing with equipment that doesn't integrate with existing systems, or facing supply chain disruptions that directly impact patient care.
For procurement managers at global healthcare institutions, the challenges multiply. You're not just sourcing equipment—you're vetting suppliers across borders, navigating different regulatory frameworks, ensuring compliance with standards like CE marking, managing complex international logistics, and trying to achieve transparent pricing in markets where information is often opaque.
This guide breaks down the entire hospital equipment procurement process into clear, actionable steps. Whether you're procuring a single device or managing a multi-million dollar capital equipment program, you'll find practical strategies to improve efficiency, reduce costs, and build a more resilient supply chain.
The Foundation: Planning and Needs Assessment
Effective hospital equipment procurement doesn't start with a purchase order; it begins with meticulous planning and a thorough needs assessment. This foundational stage is crucial for ensuring that every piece of equipment acquired aligns with our hospital's strategic goals, clinical requirements, and budgetary realities. It's where we lay the groundwork for successful Healthcare Supply Chain Management.
At this stage, we bring together a multidisciplinary team—clinicians, administrators, IT specialists, biomedical engineers, and financial experts—to collectively identify and prioritize equipment needs. This collaborative approach ensures that all perspectives are considered, from patient care and physician preference to technical integration and long-term financial viability.

The role of planning and needs assessment is to translate our healthcare requirements into future procurement needs. This involves evaluating our current equipment inventory, assessing population data, and aligning with health policies. We don't just buy what's available; we strategically acquire what's necessary to improve patient outcomes and operational efficiency.
Defining Your Hospital's Needs
Our first step in hospital equipment procurement is always to clearly define our needs. This isn't as simple as saying "we need a new MRI." It involves a detailed needs assessment, which compares our desired healthcare capabilities against our current situation, identifying any gaps. This process secures details like the precise product type, quantity, value, and intended location.
Clinical requirements are paramount. We must understand how the equipment will be used, by whom, and for which patient populations. This often involves user trials, where clinicians can test potential devices in a real-world setting, providing invaluable feedback before a final decision is made. This hands-on experience helps ensure the equipment is not only technically sound but also practical and user-friendly for our staff.
A unique aspect of healthcare procurement, compared to other industries, is the significant influence of physician preference. Doctors often act as "surrogate buyers," making the final call on which devices to use. While their expertise is vital for patient care, this can sometimes lead to cost variations. Our goal is to balance physician preferences with the overall cost-effectiveness and standardization efforts of the hospital. For instance, whether we're procuring complex diagnostic machinery or everyday Durable Medical Equipment, involving physicians early and transparently is key.
Technology and Device Evaluation
Once we understand our needs, we dive into technology assessment and device evaluation. This is where we scrutinize potential equipment to ensure it meets our exacting standards for quality, safety, and performance.
Technology assessment involves formulating an impartial, methodical, and transparent summary of the medical, social, ethical, and economic issues related to a health technology. We ask: Does this technology meet our health needs? What are its long-term implications?
Device evaluation then confirms if a device functions as intended by manufacturers. This typically involves extensive market research, often with certified facilities or laboratories, to assess a range of products. We look beyond the glossy brochures, seeking evidence of performance and reliability.
Critical to this evaluation are Technical specifications for medical devices. These specifications, often guided by international standards like those from the World Health Organization (WHO), ensure that the equipment we procure is safe, efficacious, and of high quality. Compliance with standards such as CE Marked Medical Devices is non-negotiable for equipment used in our global facilities.
We also carefully calculate the total cost of ownership (TCO). This goes beyond the initial purchase price to include installation, training, maintenance, consumables, energy consumption, and eventual decommissioning costs. Considering TCO helps us make financially sound decisions that account for the equipment's entire lifecycle. Furthermore, interoperability and IT integration are crucial. New equipment must seamlessly connect with our existing IT infrastructure and electronic health records (EHR) to avoid workflow disruptions and ensure data accuracy.
The Core Workflow of Hospital Equipment Procurement
With planning complete and needs identified, we move into the structured workflow of hospital equipment procurement. This phase transforms our strategic decisions into tangible acquisitions, following a carefully orchestrated sequence of steps from initial request to final commissioning. It’s a process that demands precision, communication, and meticulous record-keeping.

The primary components of our medical equipment procurement process include:
- People: This involves all stakeholders, from the clinicians requesting equipment to the procurement team, finance department, and IT. Their clear roles and responsibilities are vital.
- Processes: These are the established rules and procedures that guide every step, ensuring consistency and compliance.
- Paper: This encompasses all necessary documentation—requisitions, bids, contracts, invoices, and records—which are critical for accountability and auditing.
The typical workflow moves from recognizing a need, creating a purchase requisition, reviewing and approving that requisition, soliciting bids from vendors, evaluating those bids and awarding a contract, managing the order, and finally, keeping detailed records. This systematic approach ensures transparency and efficiency.
From Requisition to Purchase Order
The journey of acquiring medical equipment often begins with a purchase requisition. This is a formal document, whether written or electronic, detailing our organization's need for an item. It includes comprehensive information on the required specifications, quantity, and potential sourcing options.
Upon submission, the purchase requisition undergoes a thorough requisition review. This step involves escalation to the appropriate authorities for approval. Reviewers assess the organizational need for the equipment and, crucially, the budgetary possibilities of purchasing it. An approved requisition then formally becomes a purchase order—our commitment to acquire the item.
Following budgetary approval, we move into solicitation. This involves building a procurement plan and initiating a solicitation process, which often takes the form of a Request for Proposal (RFP) or a Request for Quotation (RFQ). We forward these requests to various vendors who can submit bids for the order. For Bulk Medical Equipment, this process can be particularly extensive, attracting multiple suppliers.
Essential information for a purchase requisition typically includes:
- Detailed description of the equipment (make, model, specifications)
- Quantity required
- Intended use and department
- Justification for the purchase
- Estimated cost
- Required delivery date
- Budget code and approval signatures
- Any necessary accessories or services (installation, training, warranty)
Installation, Commissioning, and Training
The procurement process doesn't end when the equipment arrives. The next critical stages involve installation, commissioning, and ensuring our staff are fully trained to use the new technology safely and effectively.
Installation begins with meticulous site preparation. This can involve coordinating with facilities management, engineering, and IT to ensure the designated area has the correct electrical, ventilation, and data infrastructure. Pre-dispatch inspection, sometimes conducted at the manufacturer's site, ensures the equipment meets specifications before it even leaves the factory, preventing costly delays later. Managing Medical Device Logistics for complex, often fragile, equipment requires careful planning, especially when coordinating across global supply chains.
Commissioning is a crucial phase where we run a series of tests—safety, calibration, and functionality—before the equipment is officially put into clinical use. This ensures it's safe, operating optimally, and meets all performance standards. All documentation is thoroughly checked, and any necessary adjustments are made.
Simultaneously, comprehensive staff training is conducted. This involves clinicians, technicians, and maintenance personnel, ensuring everyone understands the equipment's operation, safety protocols, and basic troubleshooting. An effective commissioning process requires a A multidisciplinary approach to medical equipment acquisition, bringing together all relevant departments to ensure a smooth transition. Finally, formal acceptance testing confirms that the equipment is installed correctly, functioning as specified, and ready for patient care.
Overcoming Key Challenges in Procurement
Even with a well-defined workflow, hospital equipment procurement is fraught with challenges. We constantly face a delicate balancing act of controlling costs while upholding the highest standards of quality and patient care. Add to this the complexities of navigating evolving regulatory landscapes and building resilient supply chains, and it's clear why procurement is a strategic imperative.
Some of the key challenges we encounter include:
- Cost variation due to supplier preferences: Physician preference items (PPIs) can lead to significant cost differences.
- Wasteful spending: Often a result of outdated data and manual processes, preventing accurate spending control.
- Hidden costs: Distribution, shipping, customs, urgent delivery fees, and inventory holding can inflate expenses.
- Specialized and customized equipment: These are often highly costly and time-consuming to procure.
- Workforce strain: Manual processes place an additional burden on our staff.
- Evolving regulatory requirements: Staying compliant across different regions is a continuous challenge.
- Supply chain fragility: The recent pandemic vividly demonstrated how disruptions can severely impact access to critical equipment.
Balancing Cost, Quality, and Clinician Preference
One of the most persistent dilemmas in hospital equipment procurement is balancing cost control with the need for top-quality equipment and respecting clinician preferences. In healthcare, unlike many other industries, physicians often have a strong voice in equipment selection due to their direct involvement in patient care. This "healthcare exceptionalism" means we can't just negotiate on price; we must also consider supplier services, training, and ultimately, patient outcomes.
This is where the concept of 'sourcing levers' becomes critical. As Eugene Schneller, a professor of supply chain management, highlights, sourcing levers are the tactical tools that translate high-level procurement strategies into actionable decisions. These include:
- Bundling purchases: Combining orders across multiple facilities within our system to achieve better pricing.
- Standardization: Reducing product variation where clinically appropriate, which simplifies support and often leads to volume discounts.
- Total Cost of Ownership (TCO) evaluation: Looking beyond the initial price to long-term costs.
- Optimizing processes with suppliers: Collaborating for efficiency.
- Building long-term partnerships: Fostering stable relationships with key Global Medical Device Distributors.
A powerful tool to steer clinician preference items (PPIs) is the value analysis committee. These multidisciplinary committees, involving clinicians, procurement, and finance, evaluate new technologies based on clinical efficacy, patient outcomes, and cost-effectiveness. For example, a physician-driven committee at Vanderbilt decreased costs of physician preference items by 11%–26% across service lines, achieving savings of greater than $8 million/year. This demonstrates that by engaging clinicians, we can achieve standardization and cost savings without compromising quality. Regular supplier performance analysis also ensures that our chosen partners consistently meet our quality and service expectations.
Navigating Regulations and Ensuring Supply Chain Resilience
In a globalized healthcare environment, navigating the complex web of regulations and building a resilient supply chain are paramount for successful hospital equipment procurement. Regulations are constantly evolving, requiring us to stay updated on Medical Regulatory Updates across all operating regions. Non-compliance can lead to significant penalties, delays, and compromise patient safety.
Our strategy for regulatory compliance involves rigorous supplier vetting. We ensure that our partners provide Certified Medical Equipment and adhere to all local and international standards. This includes verifying certifications, checking product quality, and assessing their historical performance.
The pandemic underscored the fragility of global supply chains, highlighting the critical need for resilience. Hospitals worldwide experienced shortages of essential items, forcing a re-evaluation of procurement strategies. To build resilience, we focus on:
- Risk assessment: Identifying potential points of failure in the supply chain, from manufacturing to delivery.
- Diversifying suppliers: Reducing reliance on single sources, especially for critical equipment.
- Building strong supplier relationships: Fostering trust and collaboration with key partners.
- Maintaining strategic reserves: For essential items where feasible.
- Thorough preparation: Proactive planning for potential disruptions.
These measures help us to better weather unforeseen disruptions and ensure that our patients continue to receive the care they need, regardless of external challenges.
Modernizing Procurement with Technology and Strategy
The traditional, often manual, nature of hospital equipment procurement has lagged behind the technological advancements seen in other areas of healthcare. However, the tide is turning. We are increasingly leveraging technology and strategic approaches to transform procurement from a back-office function into a strategic driver of efficiency, cost savings, and improved patient care.
The benefits of implementing an e-procurement system for medical procurement are substantial. They include reduced costs (by 5 to 7%), shorter buying cycles, elimination of bottlenecks, and increased operational efficiency. We're embracing Technology to streamline our processes, make data-driven decisions, and move towards a more value-centric approach.
The Role of Technology in Optimizing Hospital Equipment Procurement
Technology is revolutionizing how we approach hospital equipment procurement. E-procurement systems are at the forefront, automating many of the manual, paper-based processes that traditionally plague healthcare. These systems offer benefits such as:
- Reduced administrative costs: Eliminating paperwork and manual data entry.
- Faster procure-to-pay cycles: Streamlining the entire purchasing process.
- Increased transparency and audit trails: Providing clear records of all transactions.
- Better access to discounts: Through automated sourcing and negotiation tools.
We are also integrating advanced data analytics into our procurement strategies. By analyzing historical purchasing data, supplier performance, and market trends, we can make more informed decisions, identify cost-saving opportunities, and optimize inventory levels. This data allows us to track and manage information on suppliers, labor, and other expenses, leading to more efficient pricing strategies.
MedIX, for example, uses AI Medical Procurement to simplify procurement through AI-matching, rigorous compliance checks, and reliable global logistics. Our AI Smart Compare of Medical Equipment feature helps hospitals quickly identify the best options based on various criteria.
Furthermore, implementing systems like Computerized Provider Order Entry (CPOE) can significantly improve order accuracy, reducing wasted time on reordering and minimizing revenue loss due to incorrect placements. By embracing these technological advancements, we can shrink operational drag, improve efficiency, and ensure that our procurement processes are as advanced as the medical care we provide.
Shifting to Value-Based Hospital Equipment Procurement
The concept of value-based procurement represents a significant shift from traditional cost-focused approaches in healthcare. Rather than simply seeking the cheapest product, value-based procurement prioritizes long-term outcomes, patient quality of life, and the total value delivered. This means putting the patient at the center of purchasing decisions.
For example, a knee implant that costs more upfront but lasts longer and reduces the chance of revision surgery may offer greater value by improving patient quality of life and reducing overall healthcare costs in the long run. This approach moves beyond immediate savings to consider the broader impact on the healthcare system and, most importantly, on the patient.
Here's a quick comparison:
| Criteria | Cost-Focused Procurement | Value-Based Procurement |
|---|---|---|
| Primary Goal | Lowest upfront price | Optimal patient outcomes, TCO, and quality |
| Decision Factors | Purchase price, immediate budget savings | Clinical efficacy, patient safety, longevity, service, long-term costs |
| Perspective | Short-term, transactional | Long-term, strategic |
| Risk Tolerance | May accept lower quality for lower price | Prioritizes quality and minimizes long-term risks |
| Supplier Relationship | Adversarial, price-driven | Collaborative, partnership-driven |
| Evaluation Metrics | Unit cost, discount | Patient satisfaction, readmission rates, total cost of care, clinical performance |
By adopting value-based procurement, we aim to move from mere cost-cutting to value creation, benefiting patients, clinicians, and the sustainability of the healthcare system as a whole.
Frequently Asked Questions about Hospital Equipment Procurement
What is the difference between value-based and traditional cost-focused procurement?
Value-based procurement considers long-term patient outcomes, total cost of ownership, and overall value, not just the initial purchase price. It prioritizes clinical efficacy, patient safety, longevity of equipment, and the total cost of care. Traditional procurement often prioritizes the lowest upfront cost, which can lead to higher long-term expenses, compromised quality, and potentially poorer patient outcomes.
How can a hospital balance physician preference with cost control?
Balancing physician preference with cost control is a significant challenge. We address this by establishing multidisciplinary value analysis committees that include physicians, procurement specialists, and financial experts. These committees collaboratively evaluate new technologies and products, considering both clinical efficacy and cost-effectiveness. By providing clinicians with transparent data on the financial impact and patient outcomes of different devices, and by standardizing products where clinically appropriate, we can reduce costs without compromising care. As seen at Vanderbilt, this collaborative approach can lead to substantial savings, ranging from 11%–26% on physician preference items.
What are the first steps to improve our current procurement process?
To improve our current hospital equipment procurement process, we recommend starting with these actionable steps:
- Form a Multidisciplinary Team: Bring together representatives from clinical departments, finance, IT, and procurement to review existing workflows and identify pain points.
- Standardize Needs Assessment and Device Evaluation: Develop clear, consistent processes and criteria for identifying equipment needs and evaluating potential devices. This includes using technical specifications and TCO analysis.
- Implement Basic E-Procurement or Data Analytics Tools: Even a simple digital system can provide immediate insights into spending patterns, supplier performance, and bottlenecks, helping to make data-driven decisions and streamline operations.
Conclusion
Hospital equipment procurement is far more than a transactional activity; it's a strategic asset that profoundly impacts patient care, operational efficiency, and financial sustainability. From meticulous planning and needs assessment to the careful selection, installation, and ongoing management of medical devices, every step requires precision and foresight. We've seen how integrating technology, embracing value-based approaches, and fostering collaborative decision-making can transform procurement from a challenge into a competitive advantage.
By focusing on data-driven decisions, building resilient supply chains, and understanding the unique dynamics of healthcare, we can ensure our hospitals are equipped with the best tools to deliver exceptional patient outcomes. The future of hospital equipment procurement lies in smart, collaborative, and transparent processes that prioritize value and long-term success.
At MedIX, we are committed to simplifying this complex journey. As a global B2B marketplace, we connect certified medical equipment suppliers with hospitals and clinics worldwide, leveraging AI-matching, rigorous compliance checks, and reliable global logistics to ensure verified equipment and transparent transactions.
Explore how we can streamline your procurement process for buyers and sellers.
Expert voices
Insights from leaders transforming medical equipment procurement






More from our blog
Discover the latest trends in medical technology and procurement
Stay ahead of medical technology
Get the latest insights, research, and market updates delivered straight to your inbox
Ready to transform your procurement
Discover how MedIX can streamline your medical equipment sourcing process