Transforming medical equipment procurement globally

Why Healthcare Supply Chain Management is the Backbone of Patient Care
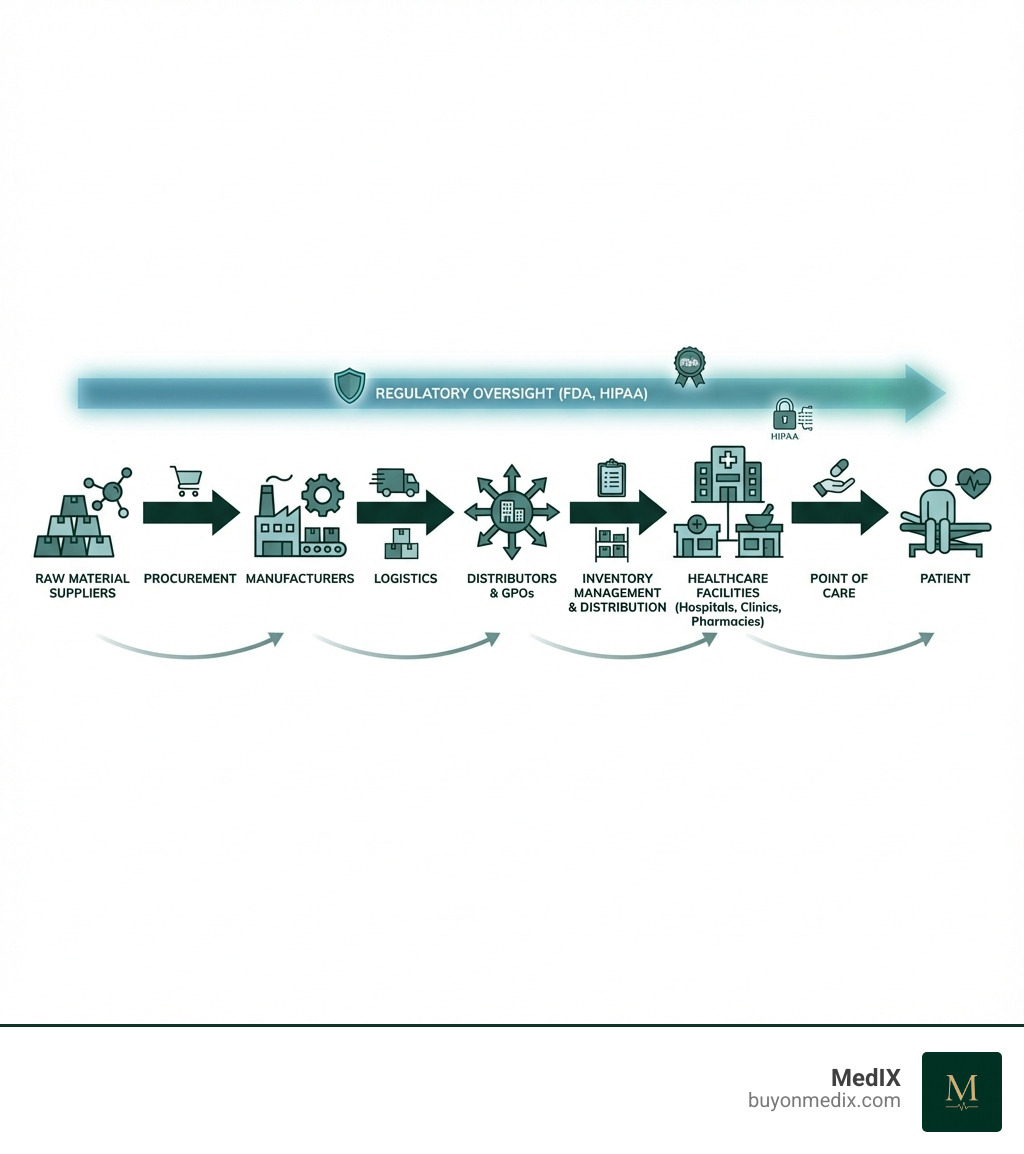
Healthcare supply chain management is the complex process of getting the right medical supplies, from Band-Aids to ventilators, to the right place at the right time. Here's what it involves:
- Procurement: Sourcing and purchasing medical supplies and equipment
- Logistics: Transporting and storing products efficiently
- Inventory Management: Tracking supplies to prevent shortouts or waste
- Distribution: Delivering items to the point of care
- Cost Control: Managing the second-largest expense for hospitals after labor
- Regulatory Compliance: Meeting FDA, HIPAA, and other requirements
Healthcare organizations need thousands of different products to deliver patient care. Because of this vast variety, their supply chains tend to be fragmented and complex. This complexity, combined with global disruptions, makes management especially challenging.
The stakes couldn't be higher. When supply chains fail, procedures get delayed or canceled. Nurses spend hours hunting for supplies instead of caring for patients. In fact, 57% of healthcare professionals can recall a time when a physician didn't have the product required for a patient's procedure.
The COVID-19 pandemic exposed just how vulnerable these systems are. Supply chain disruptions were 67% higher in 2020 than in 2019. The absence of masks and gowns was as devastating to healthcare as the semiconductor shortage that cost the automobile industry over $200 billion.
Today, the challenges persist. Nearly 80% of healthcare providers and 84% of suppliers expect supply chain challenges to worsen or remain the same over the next year. Hospital supply expenses per patient increased 18.5% between 2019 and 2022, far outpacing inflation.
For procurement managers at global healthcare institutions, these challenges are personal. You're trying to source verified medical equipment while juggling supplier vetting, compliance requirements, transparent pricing, and reliable international logistics. The complexity can feel overwhelming.
But effective supply chain management isn't just about solving logistics problems. It's about ensuring patient safety, supporting clinical staff, and maintaining financial health. When done right, it becomes a strategic competitive advantage that directly improves patient outcomes while controlling costs.
What is Healthcare Supply Chain Management and Why is it Critical?
At its heart, healthcare supply chain management involves the intricate dance of getting essential medical products and services from their point of origin to the patient. Think of it as the circulatory system of healthcare: if it’s blocked or inefficient, the whole body suffers. We're talking about everything from the simplest bandage to the most advanced surgical robot.

The core components of this vital system include:
- Procurement: This is where it all begins – the strategic sourcing and purchasing of all necessary medical supplies and equipment. It’s not just about buying; it’s about finding the right quality at the right price, globally.
- Logistics: The movement and storage of goods. This covers everything from transportation across continents to warehousing, ensuring products are kept under optimal conditions.
- Inventory Management: Keeping track of what we have, where it is, and how much we need. This delicate balance prevents both costly overstocking and dangerous shortages.
- Distribution: The final leg of the journey, getting products from warehouses to hospitals, clinics, and even directly to patients.
Why is this so critical, you ask? Because it directly impacts patient safety, the financial health of our institutions, and regulatory compliance. The supply chain isn't just a cost center; it's the second-largest expense for hospitals, right after labor. This means effective management can open up significant savings and improve the bottom line. Moreover, operating within stringent regulatory frameworks like FDA and HIPAA standards worldwide is non-negotiable.
The Core Activities of the Healthcare Supply Chain
To keep this complex system running smoothly, several core activities must be carefully managed:
- Sourcing: Identifying and evaluating potential suppliers globally, ensuring they meet our quality, compliance, and ethical standards.
- Contracting: Establishing agreements with suppliers, often through group purchasing organizations (GPOs), to secure favorable terms and prices.
- Purchasing: Placing orders and managing the procure-to-pay process, ideally with minimal manual intervention.
- Inventory Control: Monitoring stock levels, managing expiry dates, and ensuring products are stored correctly. This includes implementing systems for consignment items, especially for high-value implants.
- Warehousing: Efficiently managing storage facilities, whether centralized consolidated service centers or on-site hospital storerooms.
- Inbound/Outbound Logistics: Coordinating the movement of goods into and out of facilities, optimizing routes and carriers.
- Waste Management: Minimizing waste from expired products, damaged goods, and inefficient processes, which can be a significant cost.
Why Effective Management is a Matter of Life and Death
The consequences of a poorly managed healthcare supply chain management system are profound and can be a matter of life and death.
- Direct Impact on Patient Outcomes: When critical supplies are unavailable, patient care is directly compromised. Imagine a surgeon ready to operate, only to find a crucial device missing. An industry survey highlights this grim reality: 57% of healthcare professionals have witnessed a physician lacking a required product for a procedure. This is not just an inconvenience; it's a threat to patient safety.
- Preventing Procedural Delays: Product shortages can lead to cancelled or delayed surgeries and treatments. These delays not only impact patient health but also create significant operational inefficiencies and financial losses for healthcare providers.
- Ensuring Availability of Critical Supplies: From essential medications to life-saving equipment, the continuous availability of supplies is paramount. Without robust supply chain processes, our ability to respond to daily needs and unexpected crises is severely hampered.
- Mitigating Clinical Staff Burnout: The burden of an inefficient supply chain often falls on clinical staff. A staggering 86% of nurses surveyed admit to leaving procedures to hunt for supplies at least occasionally, with 61% stating this increases patient safety risks. This isn't just inefficient; it adds immense stress to already demanding roles, contributing to burnout.
- Reducing Risk of Using Expired Products: Manual inventory systems increase the risk of expired or recalled products remaining in circulation. 25% of nurses surveyed don't always check expiration or recall information, with nearly half (48%) attributing this to lack of time. Effective supply chain management mitigates these risks, ensuring that only safe, viable products reach our patients.
Core Challenges and Post-Pandemic Realities
Even before the COVID-19 pandemic, the healthcare supply chain management landscape was complex. Now, it's navigating a new reality shaped by persistent disruptions, escalating costs, and a heightened awareness of its vulnerabilities.

Today, we face a gauntlet of challenges:
- Supply Shortages: From everyday consumables to specialized devices, shortages remain a constant threat.
- Rising Costs: Historic inflation, increased labor costs, and liftd freight expenses continue to drive up procurement costs.
- Fragmentation: The sheer number of suppliers, products, and diverse healthcare settings (hospitals, clinics, home care) creates a fragmented system that is difficult to manage holistically.
- Lack of Visibility: Many organizations struggle with a clear, real-time view of their inventory, order status, and supplier networks.
- Data Silos: Disconnected systems and manual processes lead to inconsistent data, making informed decision-making a Herculean task.
- Drug Shortages: These are a recurring problem, often stemming from manufacturing quality issues, low profit margins for generic drugs, and market consolidation.
- Regulatory Problems: Navigating the labyrinth of global and local regulations adds layers of complexity and cost.
These challenges are not easing up. Nearly 80% of healthcare providers and 84% of suppliers expect supply chain challenges to worsen or remain the same over the next year. This statistic alone underscores the urgent need for strategic intervention.
How the COVID-19 Pandemic Exposed Deep Vulnerabilities
The COVID-19 pandemic acted as a stress test, revealing just how fragile global healthcare supply chain management systems truly were.
- PPE Shortages: We all remember the desperate scramble for personal protective equipment (PPE) like masks, gloves, and gowns. Healthcare workers on the front lines faced unimaginable risks due to insufficient supplies.
- Ventilator Scarcity: The sudden surge in demand for ventilators highlighted a critical lack of manufacturing capacity and strategic stockpiling.
- Supply Disruptions Up 67%: The pandemic triggered an unprecedented wave of disruptions, with supply chain incidents soaring by 67% in 2020 compared to 2019. This ripple effect impacted everything from raw materials to finished goods.
- Just-in-Time Inventory Failures: The efficiency-driven "just-in-time" inventory model, which minimizes warehousing costs, proved disastrous when global production lines halted and transportation networks seized up. It became clear that resilience, not just efficiency, was paramount.
- Skyrocketing Supply Costs: As demand outstripped supply, prices for essential medical items soared, putting immense financial strain on healthcare organizations already struggling with reduced elective procedures.
- Research on Supply Chain Disruptions: Academic and industry research quickly identified critical vulnerabilities, emphasizing the need for greater transparency, diversification, and strategic stockpiling.
- Semiconductor Shortage Impact: Even seemingly unrelated issues, like the global semiconductor shortage, impacted healthcare, delaying the production of critical medical devices such as pacemakers and ultrasound equipment. This demonstrated the interconnectedness of global supply chains and our reliance on upstream industries.
Ongoing Problems in a Post-COVID World
While the initial shock of the pandemic has receded, its aftershocks continue to reverberate through healthcare supply chain management.
- Historic Inflation: Persistent inflation drives up the cost of raw materials, manufacturing, and transportation, directly impacting the price of medical supplies.
- Increased Labor Costs: Staffing shortages and rising wages across the supply chain contribute to higher operational expenses.
- Continued Product Shortages: Despite lessons learned, many healthcare providers are still experiencing hundreds of different product shortages in 2024, which can negatively affect patient care.
- Geopolitical Instability: Conflicts, trade disputes, and political tensions worldwide can disrupt manufacturing, shipping routes, and access to critical resources, adding another layer of unpredictability.
- Increased Patient Treatment Costs: PwC projects a 7% increase in the cost of treating patients in the United States in 2024, continuing an upward trend. This pressure makes efficient supply chain management even more crucial.
- Hospital Supply Expenses: Hospital supply expenses per patient have increased by 18.5% between 2019 and 2022, significantly outpacing general inflation. This highlights a persistent financial strain that organizations must actively manage.
Strategies for an Optimized and Resilient Supply Chain
Navigating these persistent challenges requires a proactive, multi-faceted approach to healthcare supply chain management. We must move beyond reactive measures to build systems that are not only efficient but also robust and adaptable.
Key strategic pillars include:
- Strategic Sourcing: Shifting from transactional purchasing to building long-term, value-driven relationships with suppliers globally.
- Data Governance: Establishing clear rules and processes for managing data quality, access, and security across the entire supply chain.
- Supplier Relationships: Cultivating strong, collaborative partnerships with a diversified supplier base to improve reliability and reduce risk.
- Process Standardization: Implementing uniform procedures for procurement, inventory, and distribution to reduce errors and improve efficiency.
- Lean Principles: Applying methodologies to eliminate waste, optimize workflows, and continuously improve operations.
- Agility: Developing the capacity to respond quickly and effectively to unexpected disruptions or changes in demand.
- Resilience Planning: Proactively identifying risks and developing contingency plans to minimize the impact of future crises.
Implementing Best Practices in Healthcare Supply Chain Management
To achieve an optimized and resilient supply chain, we can implement several best practices:
- Improve Data Quality: Poor data is the enemy of efficient supply chains. We must invest in clear data governance frameworks, automated data cleansing, and regular audits to ensure accuracy.
- Automate Manual Processes: Manual procure-to-pay (P2P) and inventory management processes are prone to errors, delays, and inefficiency. Automating these workflows frees up staff, reduces costs, and improves accuracy.
- Improve System Integration: Disconnected systems create data silos. Integrating ERP, EHR, and supply chain platforms provides a holistic view, enabling better decision-making.
- Increase Supply Chain Visibility: We need end-to-end visibility, from raw material suppliers to the point of care. This means tracking inventory in real-time, monitoring shipments, and understanding supplier capacities.
- Focus on Demand Forecasting: Accurate demand forecasting is crucial to prevent both stockouts and overstocking. Leveraging historical data, clinical schedules, and predictive analytics can significantly improve our accuracy.
- Apply Lean Principles: Adopt lean methodologies to identify and eliminate waste across the supply chain. This includes reducing excess inventory, streamlining processes, and minimizing lead times. Lean inventory approaches, like just-in-time, are useful for perishable goods but must be balanced with resilience.
Building Resilience and Agility for Future Disruptions
The pandemic taught us that efficiency alone is not enough; resilience is paramount.
- Diversifying Suppliers: Relying on a single source or region for critical supplies is a major vulnerability. We must diversify our global supplier base to mitigate geopolitical risks and regional disruptions.
- Nearshoring/Onshoring: While complete onshoring may not always be feasible, exploring nearshoring or local manufacturing for certain critical items can reduce lead times and transportation risks.
- Developing Safety Stock: Strategic stockpiling of essential medical products, a departure from pure just-in-time, provides a buffer against sudden shortages. The FDA's Office of Supply Chain Resilience (OSCR) highlights the importance of such preparedness, particularly for items on the Critical Medical Device List (CMDL).
- Business Continuity Planning: Comprehensive plans detailing how to maintain operations during disruptions, including alternative sourcing, transportation, and communication strategies, are essential.
- Scenario Analysis: Regularly conducting "what-if" scenarios helps us anticipate potential disruptions and develop proactive responses.
- Creating Consolidated Service Centers (CSCs): These centralized warehouses allow for greater control over inventory, more efficient distribution, and better leverage in purchasing, especially for larger healthcare systems. They also facilitate the implementation of advanced inventory management technologies.
The Role of Technology in Modernizing Operations
The future of healthcare supply chain management is inextricably linked to technological innovation. Manual, paper-based processes and disjointed legacy systems are being replaced by digitized, automated, and cloud-based solutions that offer unprecedented visibility and control.
Cloud-based supply chain management systems, for instance, provide the scalability and interoperability needed to connect disparate parts of a vast global network. This transition is not just about efficiency; it's about changing operational decisions and improving hospital performance, as highlighted in a Harvard Business Review article on digital transformation.
Artificial Intelligence (AI), the Internet of Things (IoT), and predictive analytics are no longer futuristic concepts but essential tools enabling end-to-end visibility and proactive management.
Leveraging Technology for Improved Healthcare Supply Chain Management
Technology offers powerful solutions to many of the long-standing challenges in our supply chains:
- AI for Demand Forecasting: AI algorithms can analyze vast quantities of historical data, real-time consumption patterns, and external factors (like seasonal illness trends) to generate highly accurate demand forecasts. This helps us anticipate needs, optimize inventory levels, and even predict potential shortages before they occur. In fact, 46% of healthcare companies are already using AI to identify and address potential disruptions in their supply chains.
- IoT Sensors for Real-time Inventory Tracking: Imagine every critical medical device or high-value consumable having an IoT sensor. These sensors can provide real-time location data, temperature monitoring for sensitive items, and automated usage tracking. This eliminates manual counts and significantly reduces the risk of loss or expiration.
- RFID Scanning: Automatic Identification and Data Capture (AIDC) technologies, including barcode and RFID scanning, are becoming widespread. RFID allows for rapid, accurate tracking of items from delivery to the point of use, improving inventory accuracy and reducing manual labor for clinicians.
- Centralized Platforms for a Single Source of Truth: Cloud-based ERP (Enterprise Resource Planning) and SCM (Supply Chain Management) systems act as central hubs, integrating data from procurement, inventory, finance, and clinical systems. This creates a single, reliable source of truth, breaking down data silos and enabling comprehensive analytics.
- Digital Tools for Traceability and Anti-Counterfeiting: Technologies like blockchain offer a transparent, unalterable record of a product's journey through the supply chain. This improves traceability, helps verify authenticity, and is crucial in combating counterfeit drugs and devices, protecting patient safety.
The Foundation: Data Quality, Integration, and Visibility
The effectiveness of any technology hinges on the quality of the data it processes and the seamless integration of systems.
- Data Standardization (UDI): Standardized data is the bedrock of digital change. The FDA's Unique Device Identification (UDI) system, which assigns a unique identifier to medical devices, is a critical step. While manufacturers have populated the Global Unique Device Identification Database (GUDID), widespread adoption and utilization of UDIs throughout the healthcare supply chain remain an opportunity for improvement.
- System Interoperability: Our various systems must "talk" to each other. This means ensuring that our ERP, EHR, inventory management systems, and even supplier portals can exchange data effortlessly. This eliminates manual data entry, reduces errors, and speeds up processes.
- Real-time Dashboards: Instead of sifting through reports, real-time dashboards provide at-a-glance insights into key supply chain metrics – inventory levels, order statuses, supplier performance, and potential risks. This empowers swift, data-driven decision-making.
- Breaking Down Data Silos: Historically, departments operated with their own systems and data. Modern healthcare supply chain management demands breaking down these silos, sharing information across procurement, finance, clinical, and administrative functions to create a unified view.
- Centralized Data Platforms: Consolidating data into a single, centralized platform, often a cloud-based ERP, is essential for leveraging advanced analytics and AI. This ensures consistency and accessibility of information across the organization.
Financial Impact and Future Outlook
Effective healthcare supply chain management isn't just about operational efficiency; it's a powerful lever for financial stability and growth. Moreover, the landscape is continuously evolving, driven by technological advancements and a renewed focus on resilience and value.
Digital change in the supply chain has been shown to reduce process costs by 50% and increase revenue by 20% across many industries, and healthcare is no exception. This demonstrates a clear return on investment (ROI) for strategic supply chain initiatives.
The Financial Implications of Effective SCM
When our supply chains are well-managed, the financial benefits are substantial:
- Reducing Supply Expenses: By optimizing procurement, leveraging GPOs, and standardizing products, we can significantly lower the second-largest cost center for hospitals. Our academic commentary on SCM and health services research emphasizes how proper management practices can greatly affect medical device costs.
- Minimizing Waste: Better inventory management reduces waste from expired products, overstocking, and product damage, directly impacting the bottom line.
- Improving Contract Compliance: Ensuring that supplies are purchased at negotiated contract prices prevents unnecessary spending and maximizes the benefits of supplier agreements.
- Negotiating Better Pricing: Strong supplier relationships and data-driven insights empower us to negotiate more favorable terms and pricing globally, especially when purchasing in volume.
- Impact on Hospital Margins: In a low-margin industry where expenses are often rising faster than revenues, every dollar saved in the supply chain contributes directly to improved financial health, allowing for reinvestment in patient care and innovation.
The Future of Healthcare Supply Chain
The future of healthcare supply chain management is dynamic, promising, and strategic.
- Increased Focus on Sustainability: Beyond cost and efficiency, environmental, social, and governance (ESG) goals are gaining prominence. We will see greater emphasis on ethical sourcing, reducing carbon footprints, and supporting diverse, local suppliers. The issue of forced labor in upstream supply networks, for instance, is prompting organizations to map high-risk supply chains and craft responsible supplier contracts.
- Rise of Strategic Supply Chain Leadership: The days of the supply chain being a purely tactical function are over. Chief Supply Chain Officers (CSCOs) are increasingly recognized as C-suite executives, sitting alongside finance and clinical leaders, developing strategies that optimize clinical, operational, and financial performance.
- Deeper Clinician-Supply Chain Collaboration: The pandemic highlighted the critical need for clinicians and supply chain professionals to work hand-in-hand. Future models will involve even deeper collaboration, with clinicians providing input on product selection and supply chain leaders offering data on cost and quality. This physician engagement can lead to significant cost savings in Physician Preference Items (PPIs).
- AI-Driven Decision Making: The integration of AI will move beyond basic forecasting to predictive analytics that can anticipate complex disruptions, optimize network design, and even suggest alternative logistics options in real-time. Gartner predicts that by 2026, over 75% of commercial supply chain management applications will feature embedded AI. Our future in healthcare supply chain management will be guided by these powerful insights.
- Growth of the Healthcare SCM Market: The overall market for healthcare supply chain management solutions is expected to grow significantly, driven by the need for greater efficiency, resilience, and technological adoption. This growth reflects the industry's recognition of the supply chain as a strategic asset.
Frequently Asked Questions about Healthcare Supply Chain Management
What are the main components of a healthcare supply chain?
The main components of a healthcare supply chain management system include procurement (sourcing and purchasing medical supplies and equipment), logistics (transportation and warehousing), inventory management (tracking and storing supplies to prevent shortages or waste), and distribution (delivering items to the point of care). Beyond these physical flows, it also involves crucial elements like data management, building strong supplier relationships, and ensuring strict regulatory compliance (e.g., FDA, HIPAA).
How can technology improve healthcare supply chains?
Technology plays a transformative role in healthcare supply chain management. Artificial Intelligence (AI) can significantly improve demand forecasting and identify potential disruptions by analyzing vast datasets. The Internet of Things (IoT) sensors and RFID scanning enable real-time tracking of inventory and equipment, reducing manual effort and improving accuracy. Centralized cloud-based systems create a single source of truth for all supply chain data, breaking down silos. Digital tools, including blockchain, improve traceability, combat counterfeiting, and streamline transactions, leading to greater efficiency, visibility, and patient safety.
Why is resilience so important for the healthcare supply chain?
Resilience is paramount for the healthcare supply chain management because disruptions, as starkly revealed during the COVID-19 pandemic, can have immediate and severe impacts on patient care. Shortages of critical supplies like PPE, medications, and medical devices directly threaten patient safety and can lead to delayed or canceled procedures. A resilient supply chain is designed to better withstand and recover quickly from unexpected events such as natural disasters, geopolitical instability, or pandemics, ensuring the continuous availability of essential resources and safeguarding the continuity of care.
Conclusion
Healthcare supply chain management has evolved from a back-office function to a strategic asset, critical for patient safety, financial stability, and operational excellence. The journey towards a truly optimized and resilient healthcare supply chain is one of continuous improvement, embracing technology, and fostering deep collaboration across all stakeholders. The future of healthcare delivery depends on our collective ability to build a smart, agile, and technologically advanced supply chain that can withstand any challenge.
We understand these complexities. MedIX helps facilitate this by connecting healthcare providers with a global network of verified suppliers, simplifying procurement and enhancing supply chain reliability.
Expert voices
Insights from leaders transforming medical equipment procurement






More from our blog
Discover the latest trends in medical technology and procurement
Stay ahead of medical technology
Get the latest insights, research, and market updates delivered straight to your inbox
Ready to transform your procurement
Discover how MedIX can streamline your medical equipment sourcing process