Transforming medical equipment procurement globally

Why Medical Equipment Supplier Verification Matters for Healthcare Safety and Compliance

Medical equipment supplier verification is the systematic process healthcare organizations use to confirm that suppliers meet regulatory, quality, and safety benchmarks before purchasing critical medical devices.
Quick answer for procurement professionals:
- Verify regulatory compliance - Check FDA registration, ISO 13485 certification, and relevant premarket approvals (510(k) or PMA)
- Conduct risk assessment - Categorize suppliers based on component criticality and patient safety impact
- Review essential documentation - Request quality agreements, certificates of compliance, and audit reports
- Perform ongoing monitoring - Use supplier scorecards and scheduled audits to track performance
- Check official databases - Validate claims using FDA's registration database and AccessGUDID
A medical device is only as good as its parts. Sourcing from unverified suppliers risks receiving unapproved, unsafe, or counterfeit products. The pandemic highlighted this risk, as many hospitals received faulty or counterfeit PPE from unvetted sources, leading to financial loss and endangering healthcare workers.
The stakes are high. Working with non-credentialed or excluded vendors (e.g., one on the OIG exclusion list) presents serious financial risks, as products or services may become non-reimbursable.
Supplier verification isn't optional. It's mandated by quality management systems like the FDA's Quality System Regulations (21 CFR Part 820.50) and the global ISO 13485 standard. The Medical Device Single Audit Program (MDSAP) further streamlines compliance across multiple jurisdictions.
Many healthcare organizations struggle with inefficient verification, and expanding supply networks have increased vulnerability to unreliable partners.
This guide walks you through the complete supplier verification process, from initial screening to ongoing monitoring, so you can protect patients, ensure compliance, and build a resilient supply chain.
The Regulatory Framework for Supplier Verification
The primary purpose of medical equipment supplier verification is to ensure patient safety, product efficacy, and regulatory compliance. This diligence is integral to a manufacturer's Quality Management System (QMS), governed by global regulatory bodies and standards.
Understanding FDA Requirements
In the US, the FDA's Quality System Regulations (QSR), specifically 21 CFR Part 820.50 Purchasing Controls, mandate rigorous controls over purchased products and services.
The FDA verifies several key aspects at importation, including:
- Establishment Registration and Device Listing: US manufacturers and distributors must register annually with the FDA and list their devices. This is a crucial first step, but registration does not equal FDA approval. Use the FDA registration and listing database to verify a firm's status.
- Premarket Submission: Higher-risk devices often require premarket clearance (510(k)) or approval (PMA) before marketing.
- Compliance with Quality System Regulations: The FDA ensures manufacturers' quality systems are robust, sometimes using third-party services for onsite facility verification.
Manufacturers must diligently adhere to these regulations, maintaining clear data and quality requirements for all purchased products and services.
You can find more information about compliant equipment in our guide on Certified Medical Equipment.
Global Standards: ISO 13485 and MDSAP
Global standards provide a harmonized approach to quality management.
- ISO 13485: This international standard for medical device QMS, detailed in Section 7.4 - Purchasing, requires supplier evaluation based on their ability to meet requirements. The level of control must be proportionate to the risk.
- Medical Device Single Audit Program (MDSAP): The MDSAP allows a single audit to be recognized by multiple regulatory authorities (US, Canada, Australia, Brazil, and Japan), streamlining global market access.
- EU MDR & IVDR: In Europe, the Medical Device Regulation (EU MDR) and In Vitro Diagnostic Regulation (EU IVDR) also regulate supplier management, allowing competent authorities to conduct unannounced supplier audits, which underscores the need for continuous compliance.
Understanding these global frameworks is crucial for operating worldwide. For more insights, check out our article on Global Medical Device Distributors.
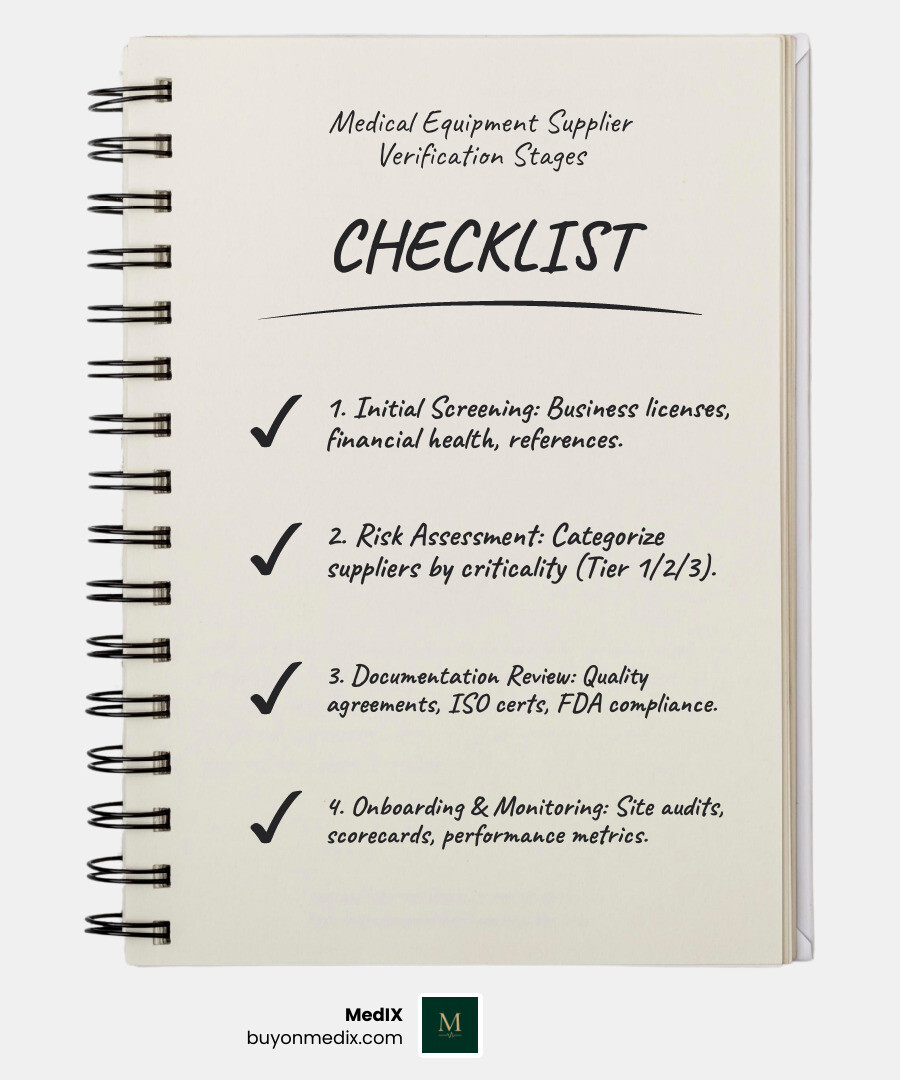
A Step-by-Step Guide to Medical Equipment Supplier Verification
Qualifying a new medical equipment supplier is a multi-stage process demanding thorough due diligence to build a robust Approved Supplier List (ASL) and safeguard your supply chain.
Step 1: Initial Screening and Qualification
Screening potential suppliers is the first step to confirm they have the foundational capabilities and legitimacy to meet your needs.
- Supplier Questionnaires: Use these to gather detailed information on a supplier's operations, QMS, manufacturing processes, and regulatory compliance history.
- Business Licenses and Financial Health Checks: Request business licenses and check financial stability. A supplier bankruptcy can disrupt critical orders. Audited financials or credit reports provide valuable insights.
- Industry References: Ask for industry references. Speaking with other organizations provides real-world insight into a supplier's reliability and quality.
- Site Visits (Virtual or Physical): For critical suppliers, an onsite audit is often non-negotiable to observe facilities, quality control, and good manufacturing practices. Virtual audits are also a viable option for initial assessments.
- Checking for Exclusions: Check the OIG and SAM exclusion lists to ensure the supplier is eligible for federal business. Transacting with an excluded entity has serious financial repercussions.
For a comprehensive checklist, refer to this FAQ and checklist to vet suppliers.
Step 2: The Role of Risk in Medical Equipment Supplier Verification
Not all suppliers and components are equal. Risk assessment helps determine the appropriate level of scrutiny for each supplier.
A risk-based approach categorizes suppliers based on their potential impact on device safety, efficacy, and quality, often using a tiered system:
- Tier 1 (High Risk): Suppliers of critical components that directly impact patient safety (e.g., specialized sensors, sterile packaging). These require intense qualification, frequent audits, robust quality agreements, and potentially a multi-sourcing strategy.
- Tier 2 (Medium Risk): Suppliers whose products have a significant but indirect impact (e.g., non-critical housing, calibration services). They require thorough qualification and regular monitoring.
- Tier 3 (Low Risk): Suppliers of "off-the-shelf" items with minimal impact (e.g., office supplies). Basic screening is sufficient.
This categorization helps allocate resources effectively. The determined level of risk informs the depth and frequency of verification activities, ensuring focus remains on critical areas.
Step 3: Essential Documentation for Medical Equipment Supplier Verification
Documentation is the backbone of compliance. Clear, traceable records for every step of the verification process provide proof of due diligence.
Essential documents to require and maintain include:
- Supplier Qualification Records: Completed questionnaires, audit reports, and approval/rejection records.
- Quality Agreements: Legally binding documents outlining quality expectations, responsibilities, and change control procedures.
- Certificates of Compliance: Certificates of Analysis (CoA), Certificates of Conformity (CoC), and declarations of compliance with regulations (e.g., RoHS, REACH).
- ISO Certifications: ISO 13485 certification (or ISO 9001 for less critical suppliers).
- FDA Records: FDA establishment registration, device listing numbers, and evidence of 510(k) clearance or PMA approval where required.
- Change Control Agreements: Agreements ensuring supplier notification of any process, material, or location changes before implementation.
- Traceability Records: Robust traceability systems for materials and components, from raw material to finished product.
- Audit Reports: Internal, third-party, and FDA 483 response audit reports.
- Product Information: Product specifications, drawings, MSDS, and relevant lab or clinical reports.
- Unique Device Identification (UDI) Information: UDI information, verifiable via the GUDID database.
This documentation is maintained within the QMS, providing objective evidence of compliance for a transparent supply chain.
Distinguishing Key Concepts: Verification vs. Validation
In medical devices, "verification" and "validation" are distinct design controls required by the FDA. Understanding the difference is key to proper medical equipment supplier verification.
| Feature | Verification | Validation |
|---|---|---|
| Purpose | Checks if the design meets specifications | Checks if the device meets user needs & intended use |
| Question | "Did you build the device right?" | "Did you build the right device?" |
| Timing | During development | After product development |
| Methodology | Reviews, inspections, bench testing | Real-world testing, clinical evaluation |
| Focus | Design output meets design input | Device specifications meet intended use |
| Output | Review reports, inspection logs, test results | Performance reports, usability study results |
Both are essential. Verification ensures the product is built to spec, while validation proves it works for its intended use. The FDA requires documentation for both activities. Neglecting these steps can lead to defects, failures, and severe consequences.
Verification: "Did you build the device right?"
Verification is a quality control process ensuring that the design output meets the design input. It answers the question, "Does the blueprint match the requirements?"
Activities involved in verification typically include:
- Reviews: Design reviews, code reviews, and documentation reviews to ensure accuracy against the Product Development Specification (PDS).
- Inspections: Physical inspections of components and processes to confirm they conform to specifications.
- Bench Testing: Performing tests in a controlled environment, such as test-firing a surgical stapler into simulated tissue to confirm its function.
- Static Analysis: Analyzing the device's design against requirements without dynamic execution.
- Documentation Review: Ensuring all design inputs and outputs are properly recorded in the Design History File (DHF).
Verification occurs throughout the development cycle, ensuring each stage correctly translates requirements into outputs.
Validation: "Did you build the right device?"
Validation confirms the finished device fulfills its intended use and user requirements in a real-world context. For example, did a surgical stapler perform effectively and safely in an actual surgery?
Validation occurs after product development is largely complete and involves:
- Functional Testing: Confirming the device operates as intended under various conditions.
- Performance Testing: Evaluating the device's ability to withstand its intended use environment, including stress and load testing.
- Clinical Evaluation/Real-World Testing: This is the ultimate test, evaluating performance in a live environment (e.g., clinical trials) with actual users to confirm factors like ergonomics and reliability on human tissue.
- Usability Studies: Ensuring the device is intuitive, safe, and effective for its intended users.
Verification ensures accuracy to spec; validation ensures effectiveness for purpose. Both are indispensable for market-ready medical equipment.
Ongoing Monitoring and Advanced Considerations
Medical equipment supplier verification is an ongoing commitment. After approval, continuous monitoring and re-evaluation are crucial for a resilient, compliant supply chain and ensuring long-term supplier quality.
Best Practices for Supplier Re-evaluation
Supplier oversight must be dynamic. Best practices for ongoing monitoring include:

- Supplier Scorecards: These are key for objective performance tracking. Scorecards track metrics like on-time delivery (FTIF), material quality, responsiveness, and Supplier Corrective Action Requests (SCARs). This data allows for weighted scoring, providing a clear performance picture.
- Scheduled Audits: Regular, scheduled audits (virtual and onsite) are non-negotiable for Tier 1 and Tier 2 suppliers to verify ongoing adherence to QMS, production, and regulatory requirements.
- Supplier Corrective Action Requests (SCARs): When nonconformities arise, SCARs are formal requests for suppliers to investigate the root cause and implement corrective actions. Tracking SCAR effectiveness is a key performance indicator.
- Managing Concession Requests: A supplier might request a "concession" for a nonconforming product. A robust supplier agreement must include a formal process for evaluating these requests, prioritizing patient safety.
- Maintaining Multiple Suppliers: For critical parts, having multiple approved suppliers mitigates risks like bankruptcy or quality issues. For single-source suppliers, consider a higher risk tier and buffer inventory to prevent disruptions.
By implementing these practices, we proactively manage risks and ensure the continuous quality of our medical equipment. For more on optimizing your supply chain, explore our insights on Medical Device Logistics.
Special Cases: Contract Manufacturers and SaMD
The evolving manufacturing landscape highlights two special cases for medical equipment supplier verification: contract manufacturers and Software as a Medical Device (SaMD) suppliers.
- Contract Manufacturers: Using contract manufacturers is common, but the legal manufacturer remains fully responsible for managing their suppliers. You can outsource work, but not responsibility. The same rigorous verification and monitoring apply, as their quality system is an extension of yours and their non-compliance reflects on you.
Software as a Medical Device (SaMD): Software is often the medical device itself (SaMD) or a critical component. SaMD suppliers include developers and providers of software-controlled instruments. Per 21 CFR 820.70(i), manufacturers must validate software for its intended use, with guidance from the FDA's "General Principles of Software Validation" (GPSV).
Software suppliers can proactively assist customers with validation by:
- Providing Comprehensive Documentation: Offering detailed product requirements, performance specifications, and limitations.
- Conducting Verification Testing: Performing and documenting their own verification tests for each software requirement.
- Making Design Control Documentation Available: Allowing customers to review design history files during audits.
- Assisting with Risk Analysis: Leveraging their expertise on instrument failure modes to help customers conduct robust risk assessments.
- Offering Validation Packages: Providing installation and operational qualification templates or full validation packages.
- Publishing Known Defect Lists: Being transparent about residual software defects allows customers to manage associated risks.
This proactive approach is a market advantage, as validation costs can exceed the instrument's purchase price. For more, see this article on software validation.
Cybersecurity: As medical devices become more connected, cybersecurity becomes an integral part of software verification and validation. Suppliers must demonstrate robust cybersecurity controls to protect patient data and device functionality.
Frequently Asked Questions about Supplier Verification
Here are answers to common questions about medical equipment supplier verification.
How do I know if a supplier's "FDA Registered" certificate is legitimate?
This is a common area for misleading claims. The truth is: The FDA does not issue "FDA Registered" or "FDA Certified" certificates to medical device facilities.
- Registration is Mandatory, Not an Endorsement: Establishments producing and distributing medical devices for the US must register annually with the FDA; this is an administrative requirement.
- Registration Does Not Mean Approval: An entry in the FDA's database does not denote approval, clearance, or authorization of a facility or its devices.
- Misleading Claims are Misbranding: Claiming "FDA Certified" for a device that isn't FDA-approved or cleared is misbranding. The FDA logo is for official use only.
To verify a supplier's registration status, always use the FDA's official database for registration and listing. Any such certificate is likely from a third party, not the FDA, and requires extreme caution.
What is a UDI and how does it help in verification?
A Unique Device Identifier (UDI) is a unique numeric or alphanumeric code with two parts:
- Device Identifier (DI): A mandatory, fixed portion identifying the device version/model and labeler.
- Production Identifier (PI): A conditional, variable portion identifying factors like lot number, serial number, and manufacturing/expiration dates.
The FDA's UDI system identifies medical devices sold in the US, from manufacturing to patient use. It's a standardized global identifier, like a barcode for medical devices.
How does it help in verification?
- Improved Traceability: UDIs allow precise device tracking through the supply chain, which is invaluable for recalls.
- Improved Post-Market Surveillance: They enable faster, more accurate adverse event reporting and clarify device performance.
- Reduced Medical Errors: They help healthcare professionals quickly identify devices, reducing errors.
- Counterfeit Detection: A verifiable UDI helps prevent counterfeit devices from entering the supply chain.
We can access device information by searching the UDI Basics from the FDA or the Global Unique Device Identification Database (GUDID).
What is the difference between a distributor and a broker?
Understanding this distinction is crucial for supplier verification and risk mitigation, especially with unfamiliar sources.
Distributors:
- Vet their suppliers.
- Take ownership of and stock products, giving them a vested interest in quality.
- Provide logistics services for proper handling and delivery.
- Build long-term relationships, fostering trust.
Brokers:
- Facilitate deals between sellers and buyers without taking ownership of products.
- Focus on transactions, not relationships.
- Brokered deals risk price gouging and lack guaranteed transport controls. Critically, some brokers deal in counterfeit products with fraudulent credentials.
Prioritize established distributors over brokers, especially in high-demand situations. If using a broker, apply rigorous verification.
Conclusion
Medical equipment supplier verification is a pillar of patient safety, financial integrity, and operational resilience. A robust process—from screening and risk assessment to documentation and monitoring—ensures every component meets the highest quality and compliance standards.
Neglecting this process leads to severe consequences like patient harm and costly recalls. A well-managed program fosters trust, streamlines procurement, and improves patient outcomes.
At MedIX, we understand these complexities. Our platform is designed to simplify procurement by connecting hospitals and clinics with certified medical equipment suppliers through AI-matching, rigorous compliance checks, and reliable global logistics. We ensure that you're always dealing with verified equipment and transparent transactions, empowering you to build a resilient and trustworthy supply chain.
Find certified suppliers and streamline your procurement process with MedIX
Expert voices
Insights from leaders transforming medical equipment procurement






More from our blog
Discover the latest trends in medical technology and procurement
Stay ahead of medical technology
Get the latest insights, research, and market updates delivered straight to your inbox
Ready to transform your procurement
Discover how MedIX can streamline your medical equipment sourcing process