Transforming medical equipment procurement globally

Why Infection Control Supplies Matter in Modern Healthcare
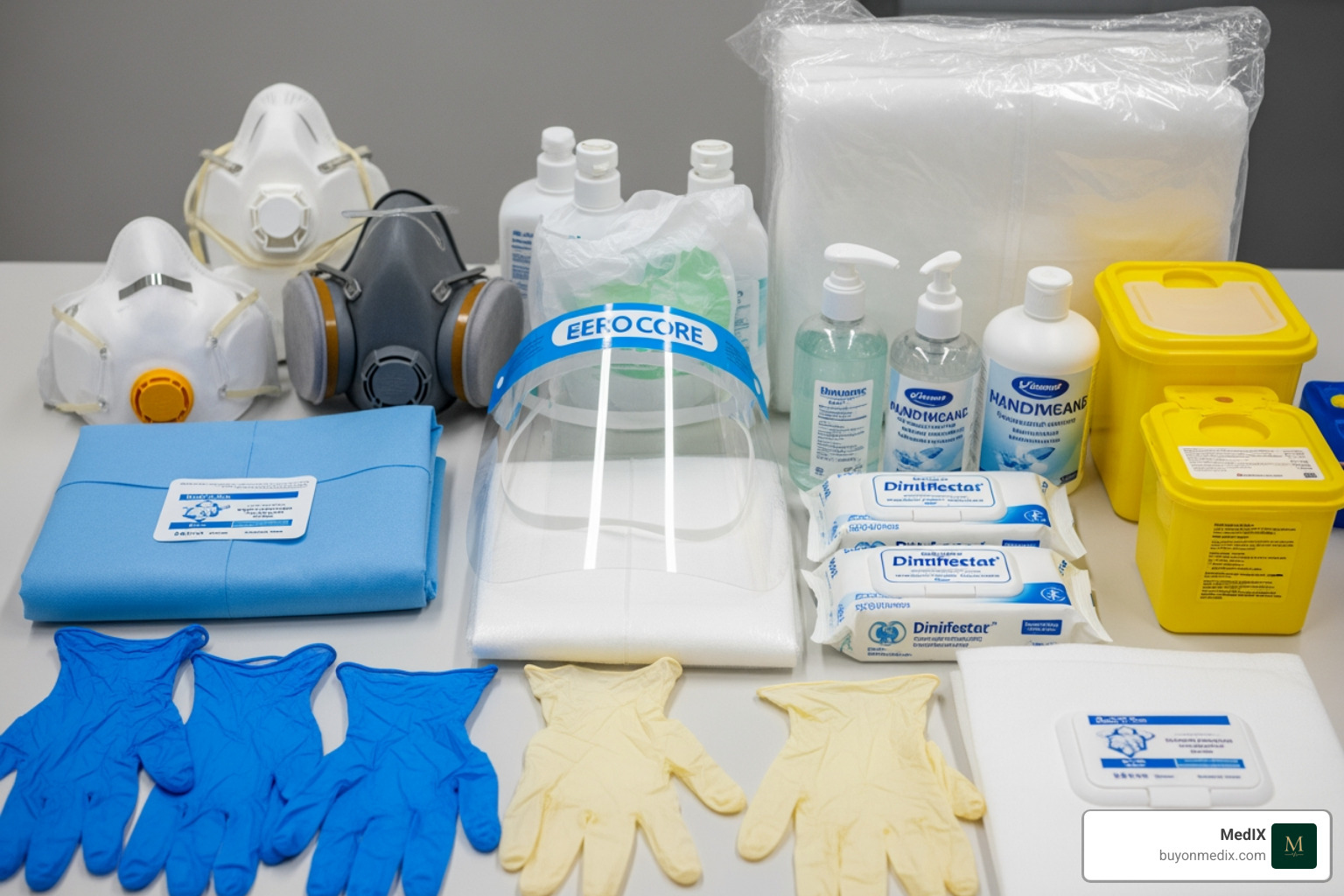
Infection control supplies are the essential tools, equipment, and materials that healthcare facilities use to prevent the spread of infectious diseases among patients, staff, and visitors. These supplies range from personal protective equipment (PPE) and hand sanitizers to disinfectants, sterilization tools, and waste disposal systems.
Quick Answer: Core Infection Control Supply Categories
- Personal Protective Equipment (PPE) - N95 respirators, nitrile gloves, isolation gowns, face shields
- Hand Hygiene Products - Alcohol-based sanitizers, surgical scrubs, skin antiseptics
- Disinfectants and Cleaners - Hospital-grade surface disinfectants, neutral detergents, sporicidal agents
- Sterilization Equipment - Autoclaves, high-level disinfection tools, reprocessing supplies
- Waste Management Systems - Sharps containers, biohazard bags, medical waste disposal units
- Environmental Cleaning Tools - Microfiber cloths, mop systems, cleaning carts
- Storage and Dispensing - Isolation stations, glove dispensers, supply carts
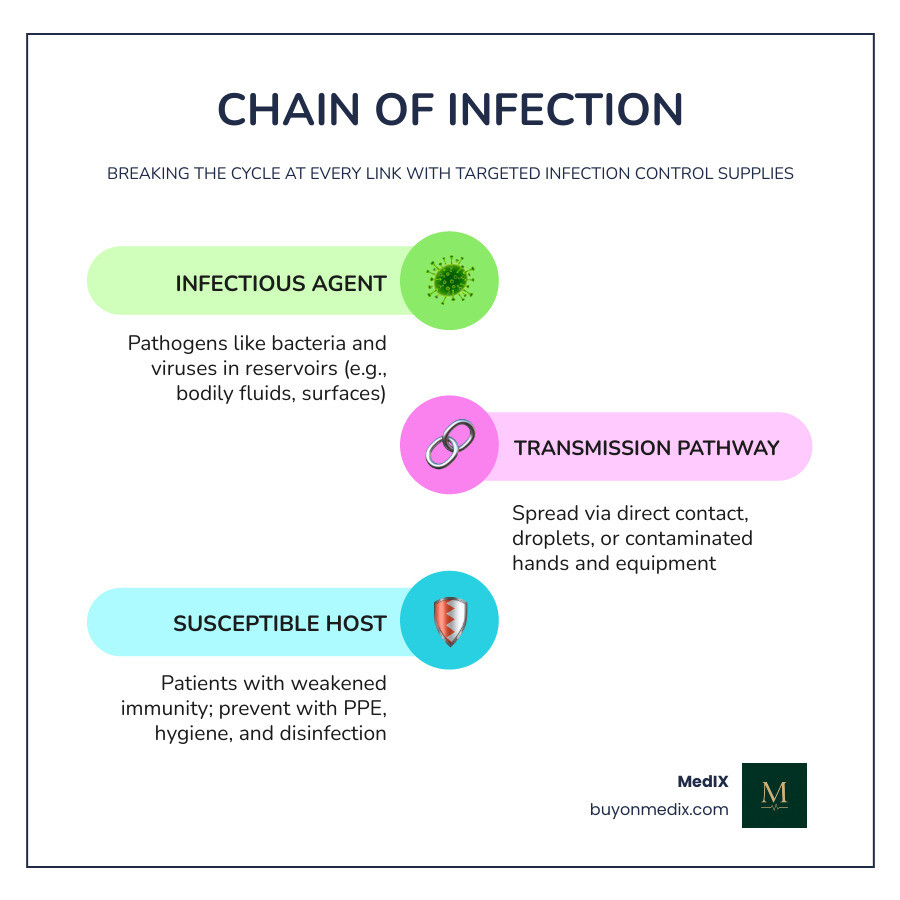
Healthcare-associated infections (HAIs) remain a persistent challenge across the globe. According to CDC guidelines, proper infection control practices using the right supplies can dramatically reduce the transmission of pathogens in clinical settings. Yet as one Alberta Health Services guideline states: "If not done properly and consistently, healthcare practices and the equipment used by healthcare providers may spread infection."
The challenge for procurement managers is not just knowing what supplies are needed, but ensuring those products meet regulatory standards, arrive on time, and come from verified suppliers. With infection prevention spanning everything from vascular access management to environmental disinfection, the supply chain must be both comprehensive and reliable.
This guide breaks down the essential categories, selection criteria, and best practices for infection control supplies in 2026, helping you build a safer healthcare environment while navigating the complexities of global medical procurement.
Learn more about infection control supplies:
Essential Categories of Infection Control Supplies
In the complex ecosystem of a hospital or clinic, infection control supplies act as the primary defense against invisible threats. We categorize these supplies into several "zones" of protection, ensuring that every touchpoint—from a surgeon's hands to the floor of an isolation room—is addressed.
The main categories include:
- Personal Protective Equipment (PPE): The physical barriers worn by staff.
- Surface Disinfectants: Chemicals used to kill pathogens on non-porous surfaces.
- Hand Hygiene: Products that remove or kill microbes on the skin.
- Waste Management: Tools for the safe containment of biohazardous materials.
When setting up a facility, it is vital to source from a reputable medical supplies supplier to ensure that every item, even specialized microbiology lab equipment, meets international safety standards like ISO or CE.
Hand Hygiene and Skin Antiseptics
Hand hygiene is often called the single most important practice for preventing the spread of germs. In 2026, we see a shift toward more "intelligent" hand hygiene systems.
- Alcohol-Based Hand Rubs (ABHR): These should ideally contain 60–80% alcohol. They are preferred for routine clinical situations unless hands are visibly soiled.
- Surgical Scrubs: Specialized antiseptics like chlorhexidine gluconate (CHG) are used for pre-operative hand preparation.
- Point-of-Care Dispensers: These should be located within arm's reach of the "patient zone" to encourage compliance.
- Skin Prep: Single-use antiseptic swabs (often iodine or CHG-based) are essential for preparing a patient's skin before injections or incisions.
Environmental Cleaning Tools
Cleaning is the necessary first step before any disinfection can occur. You can’t disinfect dirt!
- Neutral Detergents: With a pH between 6 and 8, these are the workhorses for general surface cleaning.
- Microfiber Cloths: Research shows microfiber is superior to cotton because it physically traps more microorganisms and dirt. However, be careful—high pH disinfectants (like bleach) can damage microfiber fibers over time.
- Three-Bucket Systems: A best practice for floor cleaning involves one bucket for the detergent solution, one for rinsing the mop, and a third for the disinfectant. This prevents the "redistribution of dirt" across the facility.
- Specialized Equipment: For a deep dive into the technical requirements of these tools, refer to the CDC's guide on Cleaning Supplies and Equipment.
Personal Protective Equipment (PPE) Standards and Usage
PPE is your "last line of defense." In 2026, the demand for high-quality respiratory protection remains high, with items like Moldex Latex-Free N95 Respirators often being a top priority for facilities managing airborne pathogens.
When choosing PPE, it's not just about having the items; it's about knowing how to use them. Improper Donning & Doffing Personal Protective Equipment (PPE) is a leading cause of self-contamination among healthcare workers. Whether you are stocking a large hospital or a small clinic medical supply room, the standards must remain consistent.
Respiratory Protection and Facial Barriers
Facial protection is categorized by the level of fluid resistance and filtration efficiency.
- N95 Respirators: These are NIOSH-certified and must be fit-tested. They filter at least 95% of airborne particles.
- Surgical Masks: These are evaluated based on ASTM F2100 standards (Levels 1, 2, and 3). Level 3 masks offer the highest fluid resistance, making them ideal for procedures with high splash potential.
- Face Shields: These provide an extra layer of protection for the eyes and face. While some eye protection can be reused after proper cleaning, it is vital to follow the specific protocols for the Use & Re-use of Eye Protection.
Protective Apparel and Isolation Stations
Apparel must be chosen based on the anticipated "fluid load."
- AAMI Level 3 Gowns: These are certified to provide a barrier against 16 specific types of chemotherapy drugs and high-pressure fluid splashes.
- Gown Sizing: One size does not fit all. Ensuring a range of sizes (Small to X-Large) prevents gaps in protection.
- Isolation Carts and Stations: These are centralized hubs (often mobile carts or wall-mounted organizers) that hold gloves, masks, and gowns. They should be placed right outside the door of an isolation room to ensure staff can "don" their PPE before entering the contaminated environment.
Disinfection Protocols and Device Reprocessing
Not all infection control supplies are created equal. The choice of disinfectant depends entirely on what you are trying to clean. To simplify this, we use the Spaulding Classification, which tells us the level of "kill" required based on the infection risk of the device.
Reprocessing Reusable Medical Devices
The Spaulding system divides items into three categories:
- Critical Items: These enter sterile tissue or the vascular system (e.g., surgical instruments). They must be sterilized, usually via autoclave.
- Semi-Critical Items: These contact mucous membranes or non-intact skin (e.g., endoscopes). They require high-level disinfection (HLD).
- Non-Critical Items: These only contact intact skin (e.g., stethoscopes, blood pressure cuffs). These require low-level disinfection.
For more detailed protocols, we recommend checking the Infection Control for Healthcare Providers portal.
Surface Disinfection Best Practices
When using surface disinfectants, "contact time" (or wet time) is the most critical factor. If a wipe says it has a 3-minute kill time, the surface must remain visibly wet for those full three minutes.
| Disinfectant Type | Common Use Case | Pros | Cons |
|---|---|---|---|
| Alcohol (60-80%) | Small surfaces, stethoscopes | Fast acting, no residue | Flammable, evaporates quickly |
| Chlorine (Bleach) | C. difficile, blood spills | Sporicidal, inexpensive | Corrosive, irritating odor |
| Hydrogen Peroxide | General surfaces, equipment | Safe for most surfaces | Can be expensive |
| Quaternary Ammonium | Floors, walls, furniture | Good detergent properties | Not effective against spores |
Always ensure you are using certified medical equipment and EPA/Health Canada approved chemicals to ensure the efficacy of your protocols.
Best Practices for Waste Management and Sterile Storage
Once a procedure is finished, the infection control supplies used become a potential hazard. Proper waste management is just as important as the initial disinfection.
Handling Medical Waste and Sharps
Sharps injuries are a significant risk for healthcare workers. To prevent needlesticks:
- Sharps Containers: Use puncture-resistant, leak-proof containers. Never overfill them; they should be replaced when 3/4 full.
- Color-Coded Bags: Use yellow or red biohazard liners for infectious waste. Regular trash should never be mixed with biohazard waste, as disposal costs for the latter are significantly higher.
- Safety-Engineered Devices: Whenever possible, use "self-sheathing" needles or needleless systems.
Storage Requirements for Sterile Supplies
How you store your clean supplies can be the difference between a successful surgery and a post-operative infection. We follow strict guidelines, such as those found in the AHS Infection Prevention and Control (IPC) Best Practice Recommendations, to maintain supply integrity.
- Shelving Dimensions: Shelves should be at least 25 cm (10 inches) off the floor to prevent contamination from floor cleaning. They should be 45 cm (18 inches) from the ceiling to allow for sprinkler clearance and 5 cm from outside walls to prevent moisture buildup.
- Environmental Control: Storage areas must be dry and protected from dust. If a package is dropped on the floor, it should be considered contaminated—even if there is no visible damage—as the impact can force air and bacteria into the packaging.
- Stock Rotation: Use the "First-In, First-Out" (FIFO) method to ensure supplies are used before they expire.
For facilities looking to optimize their inventory, visiting a dedicated medical equipment supply store can help identify the best storage bins and organizers for your specific space.
Frequently Asked Questions about Infection Prevention
How often should I replace infection control supplies?
Most infection control supplies like gloves, surgical masks, and isolation gowns are strictly single-use. They must be disposed of after every patient interaction or if they become visibly soiled or damp. For reusable items, follow the manufacturer’s instructions for use (MIFU). Always check expiry dates on disinfectants and sterile packaging; once a product is past its date, its efficacy cannot be guaranteed.
What is the Spaulding Classification for reusable devices?
It is a risk-assessment framework that determines how a device should be cleaned.
- Critical: High risk; requires sterilization.
- Semi-Critical: Medium risk; requires high-level disinfection.
- Non-Critical: Low risk; requires low-level disinfection.This system ensures that we don't under-clean high-risk items or over-process (and potentially damage) low-risk items.
How should sterile infection control supplies be stored?
They should be kept in a dedicated "clean" room. Shelves must be 25 cm off the floor, 45 cm from the ceiling, and 5 cm from the walls. Use impervious materials like wire or plastic rather than wood, which can harbor mold. Maintain a cleaning log for the storage area to ensure the environment remains dust-free.
Conclusion
Navigating the world of infection control supplies in 2026 requires a balance of clinical knowledge and procurement savvy. By understanding the different categories of PPE, the nuances of chemical disinfectants, and the strict requirements for sterile storage, healthcare facilities can create an environment where safety is the default setting.
At MedIX, we understand that "doing more with less" is a reality for many healthcare providers. That’s why our global B2B marketplace is designed to simplify the way you source these critical materials. We connect you with certified medical equipment suppliers through an AI-matching system that prioritizes rigorous compliance checks and reliable global logistics. Whether you are looking for N95 respirators or advanced sterilization units, we ensure that every transaction is transparent and every product is verified.
Explore the MedIX marketplace for verified medical equipment and take the guesswork out of your infection prevention program today. Together, we can build a safer future for healthcare, one sterile supply at a time.
Expert voices
Insights from leaders transforming medical equipment procurement






More from our blog
Discover the latest trends in medical technology and procurement
Stay ahead of medical technology
Get the latest insights, research, and market updates delivered straight to your inbox
Ready to transform your procurement
Discover how MedIX can streamline your medical equipment sourcing process