Transforming medical equipment procurement globally

Why ICU Medical Equipment is the Backbone of Critical Care
ICU medical equipment encompasses the life-saving devices and monitoring systems that enable intensive care units to provide 24-hour support for critically ill patients. These sophisticated tools perform essential functions: breathing for patients who cannot do so independently, delivering precise medication doses, continuously monitoring vital signs, and supporting failing organs.
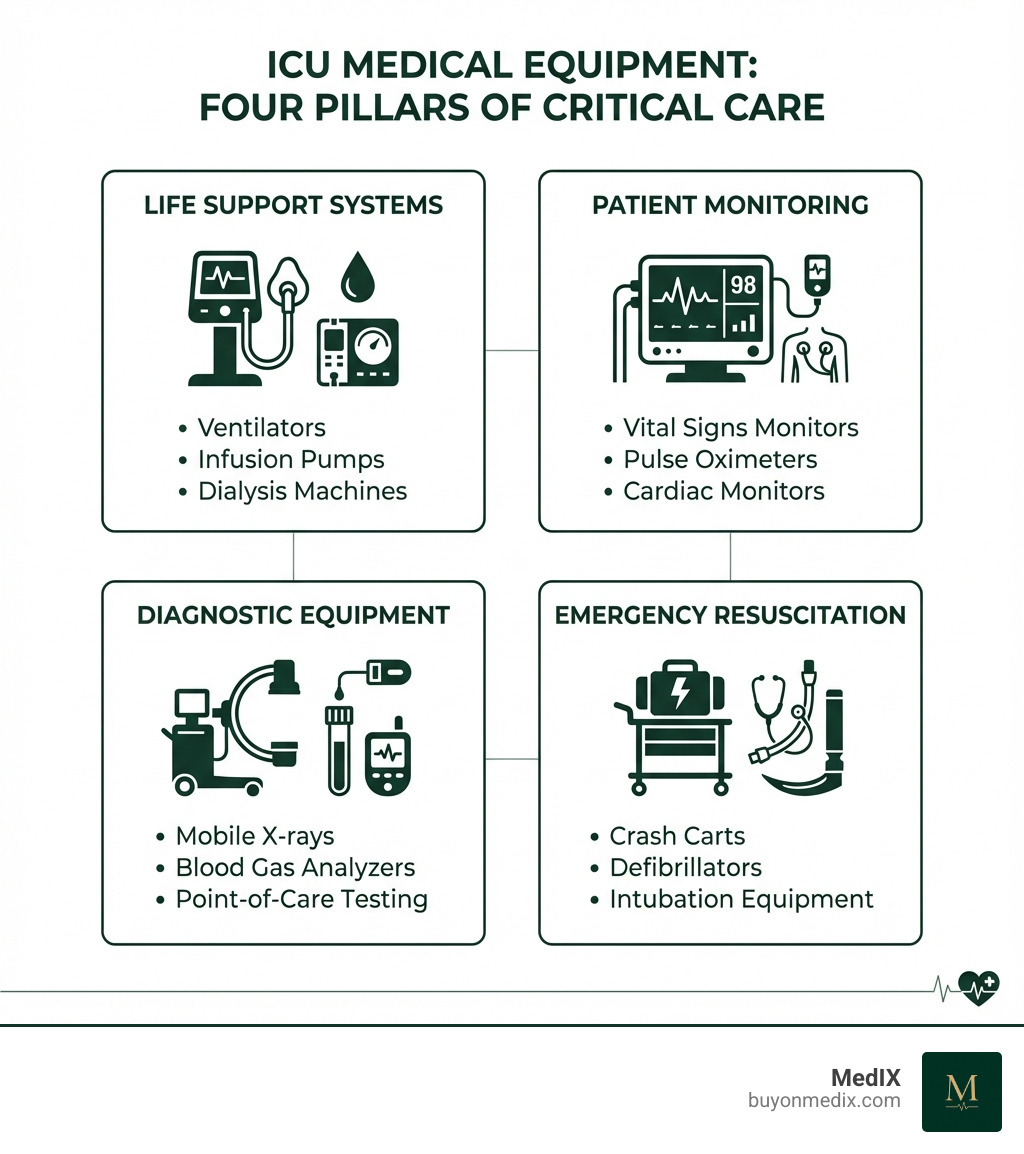
The main categories of ICU medical equipment include:
- Life Support Systems - Ventilators, CPAP machines, infusion pumps, and dialysis machines that sustain critical bodily functions
- Patient Monitoring Devices - Multi-parameter monitors, pulse oximeters, heart monitors, and blood pressure systems that track vital signs continuously
- Diagnostic Equipment - Mobile X-ray units, blood gas analyzers, and point-of-care testing devices for rapid bedside assessment
- Emergency Resuscitation Tools - Crash carts, defibrillators, and emergency intubation equipment for immediate response to life-threatening events
The global ICU devices market is projected to grow from USD 15.2 billion in 2022 to USD 23.5 billion by 2030, reflecting the critical importance of this technology. Research shows that patients in the ICU following high-risk surgery are at least three times as likely to survive when cared for by intensivists using advanced equipment.
For procurement managers, sourcing verified ICU equipment involves navigating complex challenges: ensuring regulatory compliance, vetting international suppliers, managing transparent pricing, and coordinating reliable logistics. The stakes are extraordinarily high—equipment failures or substandard devices directly impact patient survival.
This guide breaks down the essential equipment categories, explores innovations in patient monitoring and cardiology devices, and provides practical insights for operational excellence in critical care environments.
The Pillars of Life Support: Essential ICU Equipment Categories
The Intensive Care Unit (ICU) is a place where every breath, every heartbeat, and every milligram of medication can be critical. To manage these delicate balances, a complex array of specialized ICU medical equipment works in harmony, providing continuous support and intervention. This section provides a foundational understanding of the core devices that sustain life and support recovery in the ICU.
Respiratory Support Systems
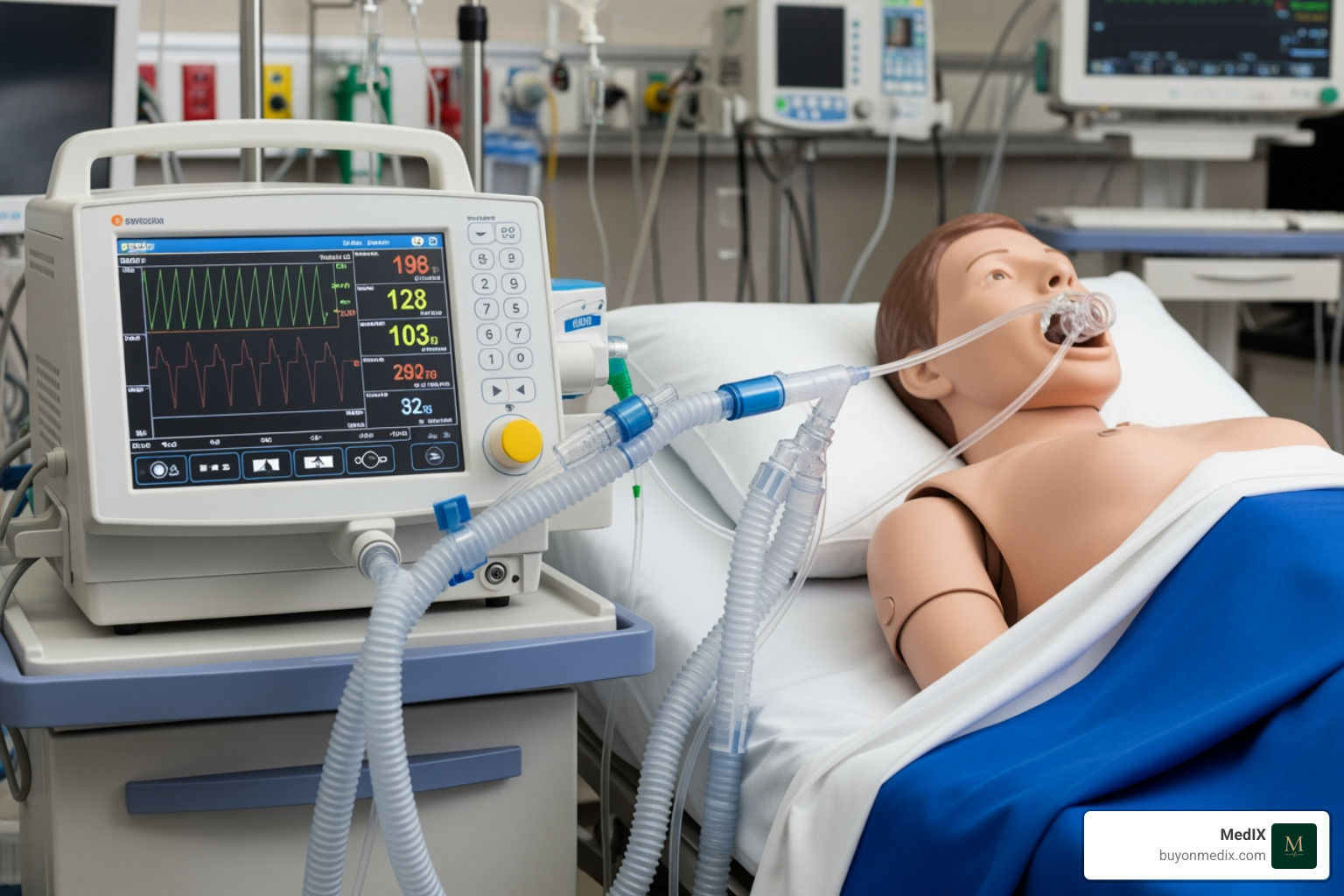
When a patient's lungs can't do their job, respiratory support systems step in as vital lifelines. These devices are designed to assist or completely take over the breathing process, ensuring adequate oxygenation and carbon dioxide removal.
- Ventilator (Mechanical Ventilator): Often the first image that comes to mind when thinking of an ICU, a ventilator is a machine that breathes for a person while their lungs are healing. It sends oxygen or air into the lungs through a tube (either an endotracheal tube or a tracheostomy tube) and allows carbon dioxide to escape. Ventilators are typically microprocessor-controlled and programmable, regulating the volume, pressure, and flow of respiration. They are used for patients with respiratory failure, which can stem from conditions like pneumonia, sepsis, or Acute Respiratory Distress Syndrome (ARDS). The global ICU ventilators market size was valued at USD 1.7 billion in 2022 and is projected to reach USD 2.7 billion by 2030, highlighting their indispensable role. For a deeper dive into their application, you can explore an overview of initiating invasive mechanical ventilation in adults in the intensive care unit.
- CPAP Machine (Continuous Positive Airway Pressure): When a full ventilator isn't needed, a CPAP machine offers a gentler form of respiratory support. It continuously pushes oxygen or air into the lungs through a mask over the nose or mouth, allowing patients to breathe on their own but with extra assistance to keep airways open. This is a common form of non-invasive ventilation (NIV).
- Nasal Cannula: For patients who only need supplemental oxygen, a nasal cannula is a simple device with two prongs placed in the nostrils. Oxygen flows through tubes directly into the nasal passages. It's used when a person just needs more oxygen, not full breathing support.
- Tracheostomy Tubes: When a patient requires long-term ventilation, or needs assistance with clearing secretions, a tracheostomy tube (often called a "trach" tube) is surgically placed directly into the windpipe. These tubes can be cuffed (to create a seal for ventilation) or uncuffed, and come in various designs, including specialized silicone tubes with features like adjustable neck flanges or talk attachments to aid communication for ventilator-dependent patients. Companies like Bivona offer a range of these specialized tubes, recognizing that one size definitely does not fit all in critical care.
Fluid, Nutrition, and Medication Delivery
Maintaining a patient's internal balance and delivering precise treatments are paramount in the ICU. A range of equipment ensures fluids, nutrition, and medications are administered safely and effectively.
- Intravenous (IV) Sites: These provide direct access to a patient's bloodstream, typically placed in a vein in the hand, arm, or foot. IV sites are crucial for delivering fluids, medications, and sometimes blood products. They also allow for blood samples to be taken for testing.
- Central Vascular Access Device (CVAD) / Central Line: A more advanced form of IV access, a CVAD is a long, thin tube inserted into a large vein, often in the neck, chest, or arm, with its tip resting near the heart. Central lines can remain in place longer than standard IVs and are used for rapid delivery of fluids, high-concentration medications, or total parenteral nutrition (TPN). They are also essential for monitoring central venous pressure.
- Infusion Pumps and Syringe Pumps: These sophisticated devices are the workhorses of medication and fluid delivery in the ICU. They deliver exactly the right amount of medicine or fluid at the right time, with extreme precision. Infusion pumps handle larger volumes, while syringe pumps are used for very small, highly controlled doses. The integration of these pumps with safety software (like LifeShield mentioned in our research) and electronic health records (EHR) is a growing trend, aiming to minimize drug errors and improve patient safety. We are seeing a strong focus on 'patient-centric' IV products and services, aiming for 'meaningful clinical differentiation' in their design and functionality.
- Gastrostomy (G-tube) and Nasogastric (NG-tube) Feeding Tubes: For patients unable to eat orally, these tubes provide essential nutrition. An NG-tube is temporarily placed through the nose into the stomach, while a G-tube is surgically inserted directly into the stomach for longer-term feeding. Beyond nutrition, they can also be used to deliver medicines or remove excess fluids from the stomach.
Diagnostic and Therapeutic Equipment
Beyond immediate life support, the ICU relies on specialized diagnostic tools for rapid assessment and therapeutic devices for specific organ support.
- Mobile X-ray Units: These portable machines allow for bedside radiography, meaning patients don't have to be moved to a radiology department for essential imaging. This is crucial for critically ill patients whose condition might be unstable.
- Point-of-Care Analyzers: These compact devices provide rapid blood chemistry results right at the bedside, much faster than sending samples to a central laboratory. This speed is invaluable in an ICU, where quick decisions based on real-time data can be life-saving.
- Dialysis Machines: For patients experiencing acute kidney injury (AKI) or chronic kidney failure, dialysis machines take over the function of the kidneys, filtering waste products and excess fluids from the blood. This is a critical therapeutic intervention in many ICU settings.
- Foley Catheter: This common device is an indwelling catheter inserted into the bladder to drain urine when a patient cannot go to the bathroom on their own. It allows for precise measurement of urine output, a key indicator of kidney function and fluid balance.
The Watchful Eye: Innovations in Patient Monitoring
Continuous monitoring is the cornerstone of intensive care, allowing for immediate response to changes in a patient's condition. In the ICU, every second counts, and these systems provide the constant vigilance needed to safeguard our most vulnerable patients.
Core Vital Signs Monitoring
At the heart of ICU care are the devices that keep a constant watch on a patient's fundamental physiological functions. The global patient monitoring systems market size was valued at USD 30.5 billion in 2022 and is expected to expand at a compound annual growth rate (CAGR) of 7.1% from 2023 to 2030, underscoring the rapid advancement and importance of this field.
- Bedside Physiologic Monitor: This multi-parameter device is the central hub for vital signs. It typically displays:
- Electrocardiogram (EKG): Tracks the electrical activity of the heart, showing heart rate and rhythm.
- Blood Pressure Monitor: Uses an inflatable cuff on the arm or leg to take regular blood pressure readings. Advanced monitors may also provide continuous arterial blood pressure monitoring.
- Pulse Oximeter: A small clip placed on a finger (or toe/earlobe) that measures how much oxygen is in the blood (SpO2 levels). This non-invasive device is crucial for assessing a patient's oxygenation status.
- Temperature Probes: Continuously monitor a patient's body temperature, which can indicate infection or other critical physiological changes.
- Respiration Rate: Monitors how many breaths a patient takes per minute, often integrated with the ventilator or EKG leads.
Advanced Hemodynamic and Neurological Monitoring
Beyond basic vital signs, some patients require more in-depth monitoring of cardiovascular function and brain activity.
- Intracranial Pressure (ICP) Monitor: For patients with severe brain injuries or conditions that cause brain swelling, an ICP monitor is surgically placed to continuously measure the pressure inside the skull. This helps clinicians prevent secondary brain damage.
- Cardiac Output Monitoring: Advanced sensors and systems can measure how much blood the heart is pumping per minute, providing critical insights into the cardiovascular system's efficiency. These can range from minimally invasive techniques to more invasive catheter-based systems.
- Advanced Sensors: Modern ICU medical equipment increasingly incorporates sophisticated sensors that provide real-time data on various physiological parameters, helping clinicians manage complex conditions like sepsis, acute kidney injury (AKI), and ARDS, especially in the context of illnesses like COVID-19. These monitoring solutions are crucial for managing ideal oxygenation and maintaining appropriate fluid balance to minimize severe life-threatening complications.
- The role of the critical care team (including intensivists, critical care nurses, and respiratory therapists) is paramount in interpreting this complex data and making informed decisions.
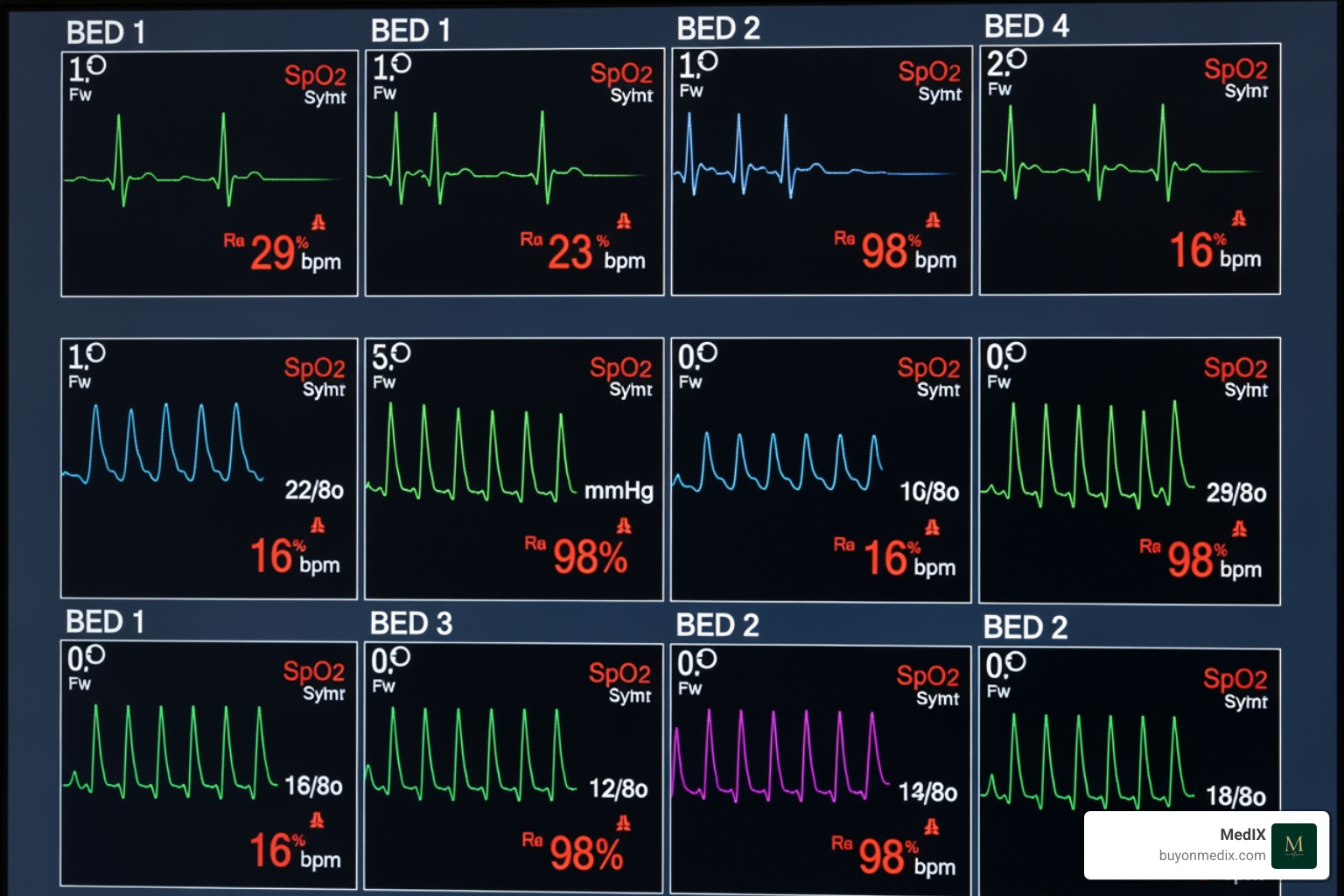
The Role of Alarms in Patient Safety
ICU medical equipment is designed with sophisticated alarm systems that serve as a critical safety net.
- Central Station Alerts: These allow caregivers to monitor multiple patients from a central location, with alarms sounding if any patient's parameters fall outside predefined safe ranges.
- Smart Alarm Systems: Modern systems are moving beyond simple "beep-beep" alarms. They aim to reduce alarm fatigue—a common issue where healthcare providers become desensitized to frequent, non-critical alarms. Smart alarm systems use algorithms to prioritize alerts, filter out false positives, and provide more context-rich warnings, ensuring that truly critical events get immediate attention.
- Prioritizing Alerts: The goal is to present clinicians with actionable information, distinguishing between a transient fluctuation and a genuine life-threatening change. This contributes significantly to patient safety protocols by ensuring timely intervention.
A Closer Look at Cardiology: Advanced ICU Medical Equipment
For patients with severe cardiac conditions, specialized ICU medical equipment provides critical heart and circulatory support, often bridging the gap until the heart can recover or other definitive treatments can be applied.
| Criterion | Intra-Aortic Balloon Pump (IABP) | Extracorporeal Membrane Oxygenation (ECMO) |
|---|---|---|
| Primary Function | Reduces heart's workload, improves coronary blood flow | Provides prolonged cardiac and/or respiratory support (artificial lung) |
| Patient Condition | Cardiogenic shock, unstable angina, post-cardiac surgery, bridge to transplant | Severe cardiac and/or respiratory failure (e.g., ARDS, severe cardiogenic shock) |
| Level of Invasiveness | Moderately invasive (catheter inserted into aorta) | Highly invasive (requires large cannulas for blood removal/return) |
Mechanical Circulatory Support
These advanced devices are deployed when the heart is too weak to adequately pump blood to the body.
- Intra-aortic Balloon Pump (IABP): The IABP is a temporary device that assists the heart by inflating and deflating a balloon in the aorta. It inflates during diastole (when the heart rests) to increase blood flow to the coronary arteries and deflates just before systole (when the heart contracts) to reduce the workload on the heart. This "heart workload reduction" helps the weakened heart pump more effectively.
- Extracorporeal Membrane Oxygenation (ECMO): ECMO is a highly advanced form of life support that acts as an artificial lung and/or heart outside the body. Blood is drawn from the patient, oxygenated by the ECMO machine, and then returned to the patient's circulation. It provides "cardiopulmonary support" for patients with severe heart or lung failure that doesn't respond to conventional treatments, buying time for the organs to recover or for other interventions.
Emergency Resuscitation Devices
Every ICU is equipped with tools for immediate response to sudden life-threatening events.
- Crash Cart (Resuscitation/Code Cart): This mobile unit is strategically stocked with essential medications, intubation equipment, and a defibrillator, ready for immediate deployment during a cardiac arrest or other medical emergency.
- Defibrillator: A device that delivers an electrical shock to the heart to restore a normal rhythm during certain types of cardiac arrest.
- Intubation Equipment: This includes laryngoscopes, endotracheal tubes, and other tools necessary to secure a patient's airway for mechanical ventilation. An overview of initiating invasive mechanical ventilation highlights the critical importance of timely and effective intubation.
- Emergency Medications: A range of drugs, such as epinephrine, atropine, and amiodarone, are readily available on the crash cart to manage acute cardiac events and other emergencies.
Specialized Cardiology-focused ICU medical equipment
Beyond the immediate life support, cardiac ICUs (CICUs) feature equipment custom for patients with complex heart conditions.
- Advanced Cardiac Monitors: These monitors offer more detailed analysis of heart function, including continuous 12-lead EKGs, advanced arrhythmia detection, and sometimes even direct measurement of cardiac pressures.
- Temporary Pacemakers: For patients with dangerously slow heart rates or certain heart blocks, temporary pacemakers can deliver electrical impulses to stimulate the heart and maintain a stable rhythm.
- Post-cardiac Surgery Care: After complex heart surgeries, patients require intensive monitoring and support from specialized ICU medical equipment to ensure hemodynamic stability and manage potential complications.
Operational Excellence: Managing and Maintaining Critical Care Technology
The sheer volume and complexity of ICU medical equipment mean that optimal operation and rigorous maintenance are not just best practices—they are necessities. Ensuring equipment reliability, staff efficiency, and, ultimately, patient safety hinges on these considerations.
Key Considerations for Operation and Maintenance
The seamless functioning of an ICU is a testament to meticulous planning and execution in equipment management.
- Staff Training: The most advanced equipment is only as good as the people operating it. All ICU staff, including nurses, respiratory therapists, and physicians, must undergo specialized training in critical care and be proficient in operating the various devices. Manufacturers often provide comprehensive training for sophisticated equipment. This continuous education ensures that clinicians are not only familiar with the controls but also understand the underlying principles and potential pitfalls.
- Daily Equipment Checks: Proactive vigilance is key. Daily checks on all ICU medical equipment are essential to confirm proper functionality, calibrate settings, and identify any issues before they become critical.
- Sterilization Protocols: To prevent healthcare-associated infections, rigorous disinfection and sterilization protocols for all reusable patient care equipment are non-negotiable. Disposable items must also be discarded correctly in properly labeled containers.
- Biomedical Engineering: This unsung hero department is the backbone of equipment maintenance. Biomedical engineering staff are responsible for routine maintenance, prompt repairs, and ensuring all devices meet safety and performance standards.
- Preventive Maintenance Contracts: For complex and expensive devices, maintaining current service and preventive maintenance contracts is crucial. These contracts ensure regular inspections and servicing by qualified technicians, minimizing downtime and extending equipment lifespan.
- Regulatory Compliance: All ICU medical equipment must adhere to strict national and international regulatory standards. Procurement teams, like ours, ensure that all sourced equipment meets these rigorous compliance checks, providing peace of mind to hospitals and clinics worldwide.
Adapting ICU medical equipment for Specialized Units
While a core set of ICU medical equipment is universal, specialized units within the intensive care spectrum adapt their technology to meet unique patient populations' needs.
- Neonatal ICU (NICU): Caring for the smallest and most vulnerable patients, NICUs require highly specialized equipment. This includes incubators for precise temperature and humidity control, ventilators designed for extremely low tidal volumes and delicate lungs, and monitors with algorithms sensitive to neonatal vital signs. The National Association of Neonatal Nurses (NANN) plays a crucial role in advancing best practices in this specialized field.
- Pediatric ICU (PICU): For infants, children, and adolescents, PICUs use size-specific devices—smaller catheters, appropriately sized breathing circuits, and medication pumps capable of delivering micro-doses.
- Trauma ICU and Burn Units: These units are equipped for rapid stabilization and ongoing care of severe injuries. They often have specialized wound care equipment, advanced fluid resuscitation systems, and robust monitoring capabilities to handle complex physiological responses to trauma or extensive burns.
- Cardiac ICU (CICU): As discussed, CICUs feature advanced cardiac monitors, temporary pacemakers, and mechanical circulatory support devices like IABPs and ECMO, custom for patients with acute heart conditions.
Ensuring Patient Safety and Comfort
Beyond the technical efficacy, modern ICU medical equipment and unit design are increasingly focusing on the patient experience. How does this equipment contribute to patient safety and comfort?
- Ergonomic Design: Equipment is designed to be intuitive for staff to operate, reducing the potential for errors. This includes clear displays, logical controls, and easy-to-access components.
- Noise Reduction Strategies: The ICU can be a cacophony of alarms and machine sounds, contributing to patient delirium and stress. The concept of a 'Quiet ICU' is gaining traction, with efforts to reduce ambient noise through quieter equipment, smart alarm systems, and acoustic design.
- Specialized ICU Beds: These are not just ordinary beds. They are often equipped with features like automated positioning, built-in scales, and pressure-reducing mattresses to prevent pressure ulcers, improve patient comfort, and facilitate nursing care.
- Patient Positioning Systems: Devices and protocols ensure proper patient positioning, which is vital for preventing complications like pneumonia, improving ventilation, and managing pressure points. These systems contribute directly to "pressure ulcer prevention" and overall well-being.
Frequently Asked Questions about ICU Medical Equipment
What are the most critical pieces of equipment in a standard ICU?
The most critical equipment includes mechanical ventilators for breathing support, multi-parameter patient monitors for tracking vital signs (heart rate, blood pressure, oxygen saturation), and infusion pumps for precise delivery of medications and fluids. These form the core of life support and continuous observation.
How does equipment selection differ for a specialized unit like a NICU?
Equipment for a Neonatal ICU (NICU) is highly specialized. Devices are significantly smaller and designed for the unique physiology of premature and full-term infants. This includes specialized ventilators with lower tidal volumes, incubators for temperature regulation, and monitors with algorithms sensitive to neonatal vital signs.
What is the importance of equipment interoperability in the ICU?
Interoperability—the ability of different devices to connect and share data—is crucial in a modern ICU. It allows for the creation of a comprehensive electronic health record (EHR), reduces manual charting errors, enables smart alarms that analyze data from multiple sources, and provides clinicians with a complete, real-time picture of the patient's status to improve decision-making.
Conclusion: Sourcing the Future of Critical Care
The sophisticated array of ICU medical equipment, from life-sustaining ventilators to advanced cardiac monitors, represents the pinnacle of medical technology. These integrated systems are fundamental to providing high-level care and improving outcomes for the most vulnerable patients. Ensuring access to reliable, certified, and technologically advanced equipment is a critical challenge for healthcare facilities worldwide. For hospitals and clinics looking to procure verified critical care technology, MedIX provides a streamlined and trusted global marketplace. We simplify procurement through AI-matching, rigorous compliance checks, and reliable global logistics, ensuring verified equipment and transparent transactions worldwide. Explore a comprehensive range of ICU medical equipment categories to equip your facility for excellence in patient care.
Expert voices
Insights from leaders transforming medical equipment procurement






More from our blog
Discover the latest trends in medical technology and procurement
Stay ahead of medical technology
Get the latest insights, research, and market updates delivered straight to your inbox
Ready to transform your procurement
Discover how MedIX can streamline your medical equipment sourcing process